合成生物学 ›› 2024, Vol. 5 ›› Issue (4): 770-781.DOI: 10.12211/2096-8280.2023-095
睾丸类器官在体外精子发生中的研究进展
张博航, 祁晓萱, 袁艳
- 南京医科大学生殖医学与子代健康全国重点实验室,江苏 南京 211166
-
收稿日期:2023-11-30修回日期:2024-03-05出版日期:2024-08-31发布日期:2024-09-19 -
通讯作者:袁艳 -
作者简介:张博航 (1999—),男,博士研究生。研究方向为精子发生过程中相关机制。E-mail:zhangbohang2018@163.com袁艳 (1987—),女,博士,教授,博士生导师。研究方向为体外男性生育力重构,包括胚胎干细胞(ESC)和诱导多能干细胞(iPSC)分化、睾丸类器官重构及相关机制。E-mail:yuanyan@njmu.edu.cn -
基金资助:国家重点研发计划(2022YFC2702800);国家自然科学基金(82122025)
Advancements in testicular organoids for in vitro spermatogenesis
ZHANG Bohang, QI Xiaoxuan, YUAN Yan
- State Key Laboratory of Reproductive Medicine and Offspring Health,Nanjing Medical University,Nanjing 211166,Jiangsu,China
-
Received:2023-11-30Revised:2024-03-05Online:2024-08-31Published:2024-09-19 -
Contact:YUAN Yan
摘要:
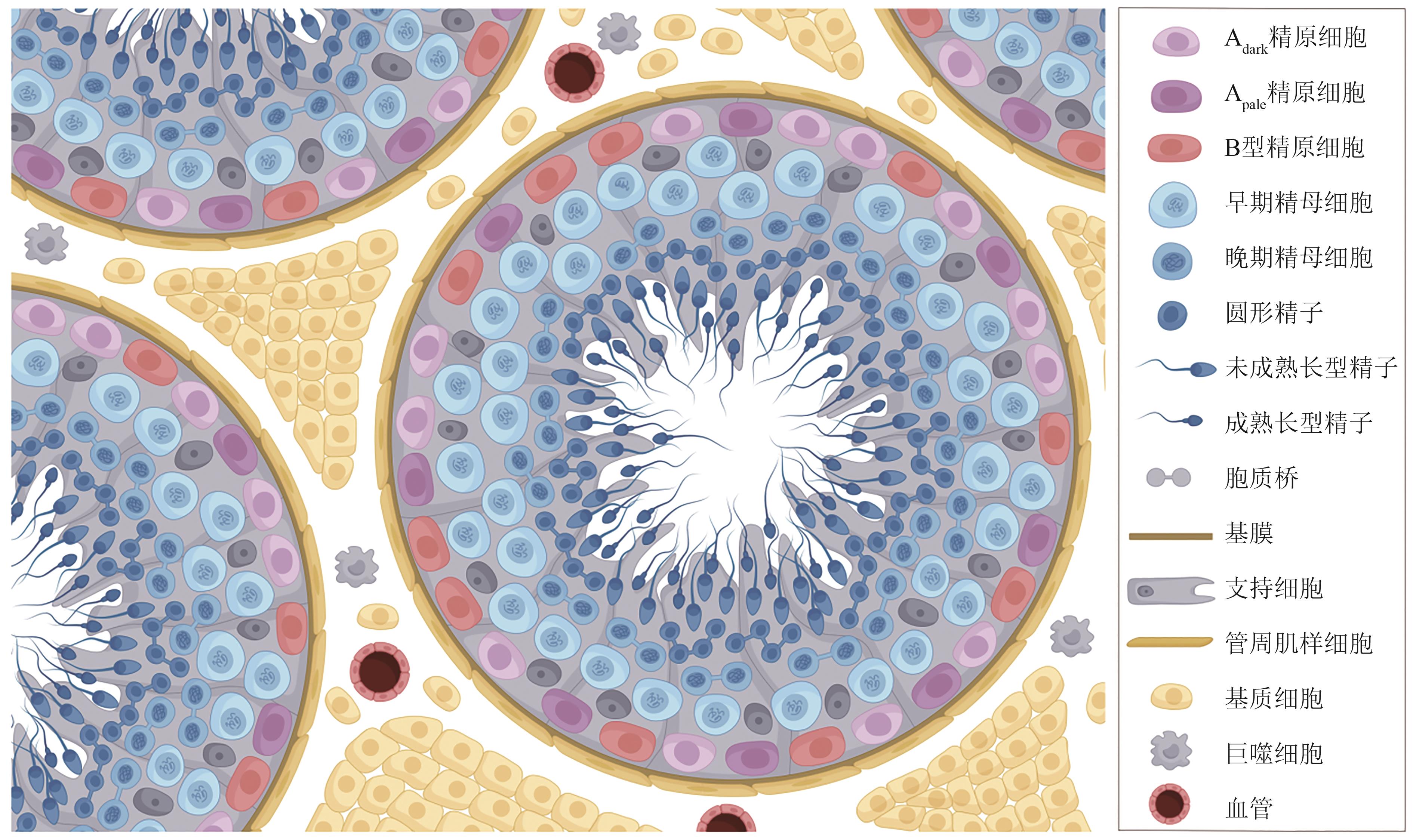
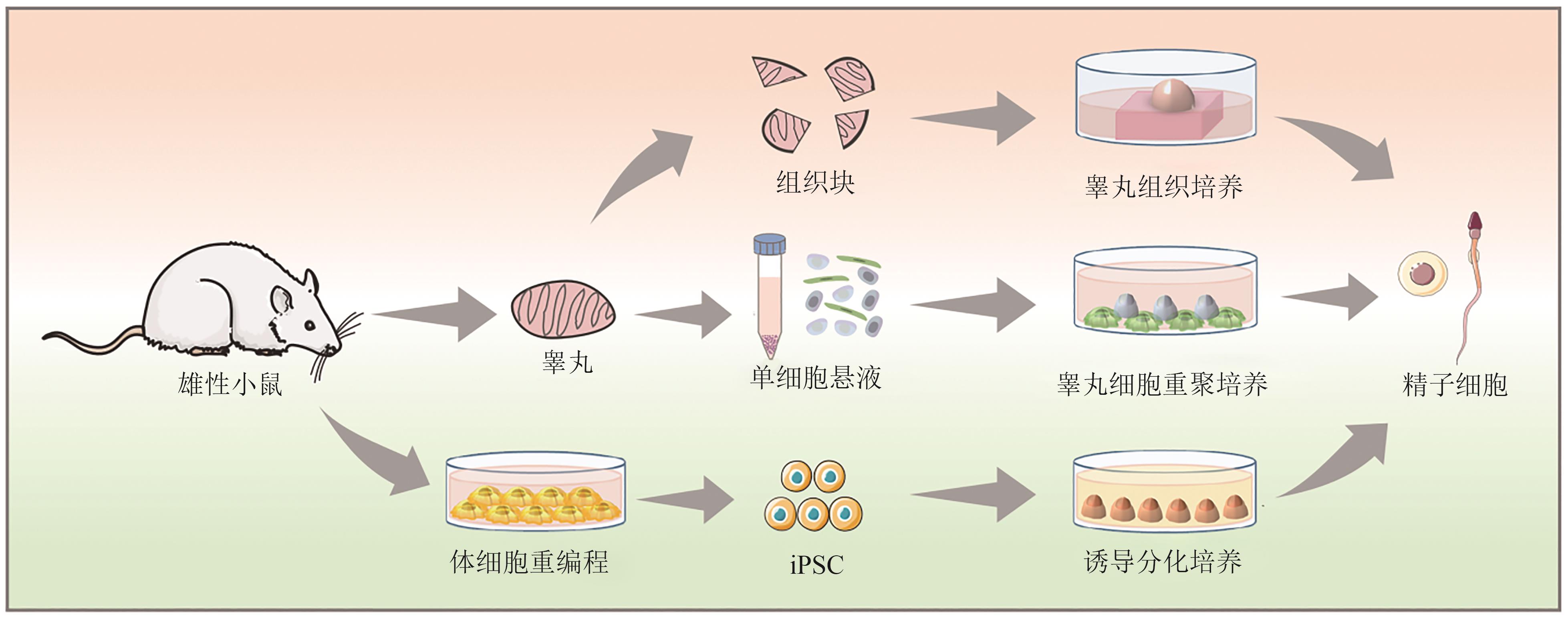
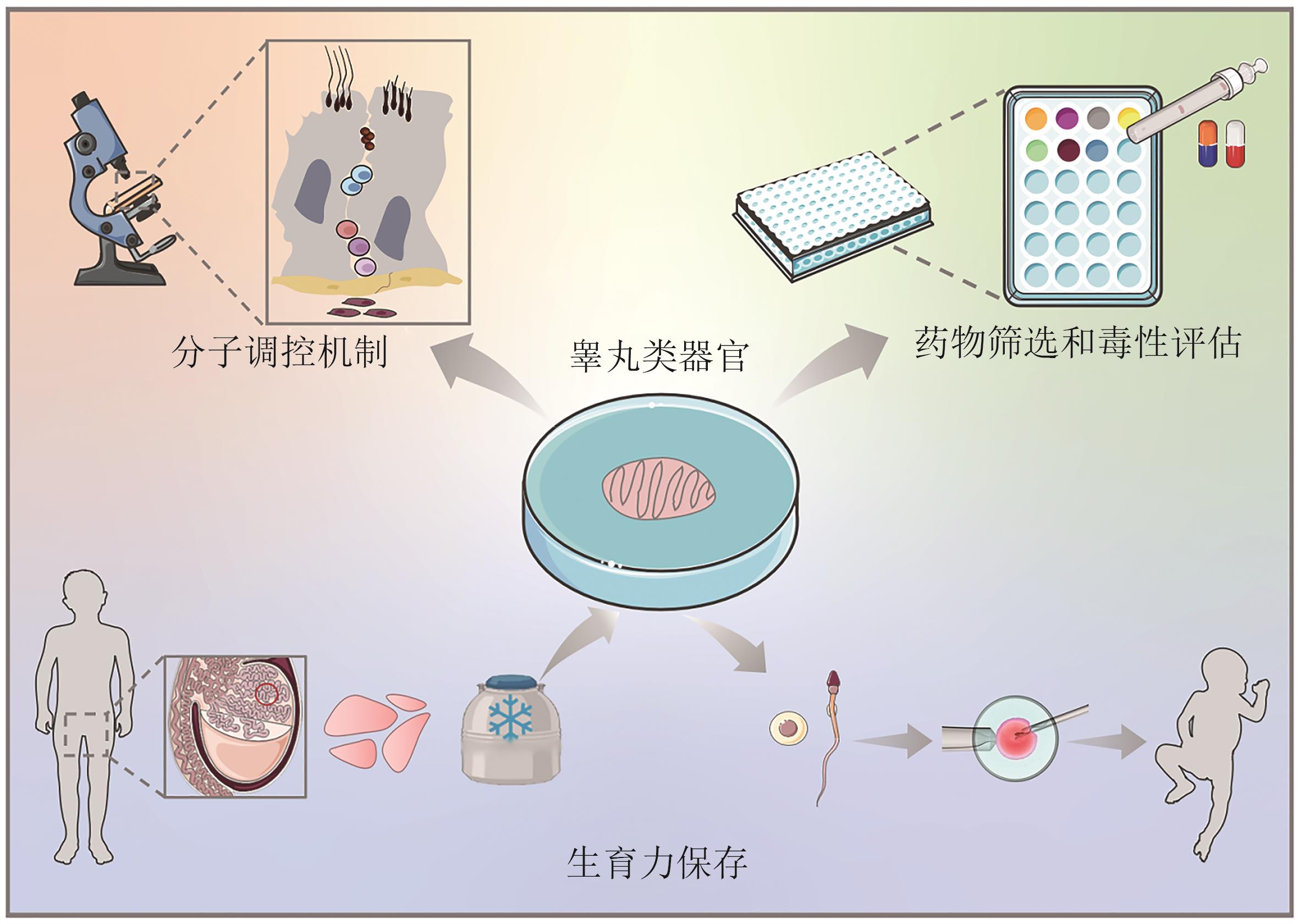
随着全球不孕不育问题的日益严重,特别是男性不育症的比例逐年上升,睾丸类器官的研究为这一领域提供了新的希望和策略。本综述全面探讨了睾丸类器官在模拟自然生精环境、深入探究精子发生机制以及应对男性生殖健康挑战中的应用。首先,介绍了睾丸的生理功能和精子发生过程的重要性,关注了睾丸组织体外培养和睾丸细胞重聚类器官的技术及其研究进展。其次,探讨了睾丸类器官在探究分子机制、药物筛选和毒性评估及男性生育力保存方面的潜在应用。最后,对当前方法的局限性和未来研究方向进行了讨论,特别是在提高体外环境下精子质量和成熟度方面的研究成果。尽管睾丸微环境复杂,在体外完整模拟人类精子发生仍面临挑战,但睾丸类器官领域的不断发展有望为临床生殖医学和男性健康研究提供新的解决方案。
中图分类号:
引用本文
张博航, 祁晓萱, 袁艳. 睾丸类器官在体外精子发生中的研究进展[J]. 合成生物学, 2024, 5(4): 770-781.
ZHANG Bohang, QI Xiaoxuan, YUAN Yan. Advancements in testicular organoids for in vitro spermatogenesis[J]. Synthetic Biology Journal, 2024, 5(4): 770-781.
| 1 | GRISWOLD M D. Spermatogenesis: the commitment to meiosis[J]. Physiological Reviews, 2016, 96(1): 1-17. |
| 2 | DU L, CHEN W, CHENG Z X, et al. Novel gene regulation in normal and abnormal spermatogenesis[J]. Cells, 2021, 10(3): 666. |
| 3 | OKONOFUA F E, NTOIMO L F C, OMONKHUA A, et al. Causes and risk factors for male infertility: a scoping review of published studies[J]. International Journal of General Medicine, 2022, 15: 5985-5997. |
| 4 | AGARWAL A, BASKARAN S, PAREKH N, et al. Male infertility[J]. Lancet, 2021, 397(10271): 319-333. |
| 5 | INHORN M C, PATRIZIO P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century[J]. Human Reproduction Update, 2015, 21(4): 411-426. |
| 6 | NJAGI P, GROOT W, ARSENIJEVIC J, et al. Financial costs of assisted reproductive technology for patients in low- and middle-income countries: a systematic review[J]. Human Reproduction Open, 2023, 2023(2): hoad007. |
| 7 | MCLACHLAN R I. Approach to the patient with oligozoospermia[J]. The Journal of Clinical Endocrinology and Metabolism, 2013, 98(3): 873-880. |
| 8 | SHAHROKHI S Z, SALEHI P, ALYASIN A, et al. Asthenozoospermia: cellular and molecular contributing factors and treatment strategies[J]. Andrologia, 2020, 52(2): e13463. |
| 9 | WOSNITZER M, GOLDSTEIN M, HARDY M P. Review of azoospermia[J]. Spermatogenesis, 2014, 4: e28218. |
| 10 | Practice Committee of the American Society for Reproductive Medicine in Collaboration with the Society for Male Reproduction and Urology. The management of obstructive azoospermia: a committee opinion[J]. Fertility and Sterility, 2019, 111(5): 873-880. |
| 11 | PICTON H M, WYNS C, ANDERSON R A, et al. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys[J]. Human Reproduction, 2015, 30(11): 2463-2475. |
| 12 | ALIAKBARI F, TAGHIZABET N, AZIZI F, et al. A review of methods for preserving male fertility[J]. Zygote, 2022, 30(3): 289-297. |
| 13 | HEZAVEHEI M, SHARAFI M, KOUCHESFAHANI H M, et al. Sperm cryopreservation: a review on current molecular cryobiology and advanced approaches[J]. Reproductive Biomedicine Online, 2018, 37(3): 327-339. |
| 14 | FATEHULLAH A, TAN S H, BARKER N. Organoids as an in vitro model of human development and disease[J]. Nature Cell Biology, 2016, 18(3): 246-254. |
| 15 | MCCAULEY H A, WELLS J M. Pluripotent stem cell-derived organoids: using principles of developmental biology to grow human tissues in a dish[J]. Development, 2017, 144(6): 958-962. |
| 16 | 李娟娟, 张君涛, 赵英博, 等. 类器官的研究进展及应用前景[J]. 中国畜牧兽医, 2021, 48(6): 1985-1994. |
| LI J J, ZHANG J T, ZHAO Y B, et al. Research progress and application prospect of organoids[J]. China Animal Husbandry & Veterinary Medicine, 2021, 48(6): 1985-1994. | |
| 17 | QUADRATO G, NGUYEN T, MACOSKO E Z, et al. Cell diversity and network dynamics in photosensitive human brain organoids[J]. Nature, 2017, 545(7652): 48-53. |
| 18 | TAKEBE T, SEKINE K, ENOMURA M, et al. Vascularized and functional human liver from an iPSC-derived organ bud transplant[J]. Nature, 2013, 499(7459): 481-484. |
| 19 | TAKEBE T, ZHANG R R, KOIKE H, et al. Generation of a vascularized and functional human liver from an iPSC-derived organ bud transplant[J]. Nature Protocols, 2014, 9(2): 396-409. |
| 20 | SCHMIDT C, DEYETT A, ILMER T, et al. Multi-chamber cardioids unravel human heart development and cardiac defects[J]. Cell, 2023, 186(25): 5587-5605.e27. |
| 21 | BOJ S F, HWANG C I, BAKER L A, et al. Organoid models of human and mouse ductal pancreatic cancer[J]. Cell, 2015, 160(1/2): 324-338. |
| 22 | MORGAN J P, DELNERO P F, ZHENG Y, et al. Formation of microvascular networks in vitro [J]. Nature Protocols, 2013, 8(9): 1820-1836. |
| 23 | WANG N Z, SHEN J M, MINGHUA L I U, et al. A brief history of testicular organoids: from theory to the wards[J]. Journal of Assisted Reproduction and Genetics, 2022, 39(7): 1423-1431. |
| 24 | 张栋, 杜黎, 何祖平. 男性生殖系统类器官的研究进展[J]. 湖南师范大学学报(医学版), 2022, 19(4): 1-6. |
| ZHANG D, DU L, HE Z P. Research advancement on the organoids of male reproductive system[J]. Journal of Hunan Normal University (Medical Sciences), 2022, 19(4): 1-6. | |
| 25 | SVINGEN T, KOOPMAN P. Building the mammalian testis: origins, differentiation, and assembly of the component cell populations[J]. Genes & Development, 2013, 27(22): 2409-2426. |
| 26 | MÄKELÄ J A, KOSKENNIEMI J J, VIRTANEN H E, et al. Testis development[J]. Endocrine Reviews, 2019, 40(4): 857-905. |
| 27 | 朱文倩, 蔡宁宁, 杨蕊, 等. 精子发生研究进展[J]. 生命科学, 2020, 32(10): 1021-1028. |
| ZHU W Q, CAI N N, YANG R, et al. Advances in spermatogenesis[J]. Chinese Bulletin of Life Sciences, 2020, 32(10): 1021-1028. | |
| 28 | GRISWOLD M D. The central role of Sertoli cells in spermatogenesis[J]. Seminars in Cell & Developmental Biology, 1998, 9(4): 411-416. |
| 29 | LUACES J P, TORO-URREGO N, OTERO-LOSADA M, et al. What do we know about blood-testis barrier? Current understanding of its structure and physiology[J]. Frontiers in Cell and Developmental Biology, 2023, 11: 1114769. |
| 30 | CHEN L Y, BROWN P R, WILLIS W B, et al. Peritubular myoid cells participate in male mouse spermatogonial stem cell maintenance[J]. Endocrinology, 2014, 155(12): 4964-4974. |
| 31 | MAEKAWA M, KAMIMURA K, NAGANO T. Peritubular myoid cells in the testis: their structure and function[J]. Archives of Histology and Cytology, 1996, 59(1): 1-13. |
| 32 | ZIRKIN B R, PAPADOPOULOS V. Leydig cells: formation, function, and regulation[J]. Biology of Reproduction, 2018, 99(1): 101-111 |
| 33 | MEINHARDT A, WANG M, SCHULZ C, et al. Microenvironmental signals govern the cellular identity of testicular macrophages[J]. Journal of Leukocyte Biology, 2018, 104(4): 757-766. |
| 34 | TAN K, SONG H W, WILKINSON M F. Single-cell RNAseq analysis of testicular germ and somatic cell development during the perinatal period[J]. Development, 2020, 147(3): dev183251. |
| 35 | O’DONNELL L, SMITH L B, REBOURCET D. Sertoli cells as key drivers of testis function[J]. Seminars in Cell & Developmental Biology, 2022, 121: 2-9. |
| 36 | ROBINSON M, SPARANESE S, WITHERSPOON L, et al. Human in vitro spermatogenesis as a regenerative therapy—where do we stand?[J]. Nature Reviews Urology, 2023, 20(8): 461-479. |
| 37 | MCLAREN A. Primordial germ cells in the mouse[J]. Developmental Biology, 2003, 262(1): 1-15. |
| 38 | FAYOMI A P, ORWIG K E. Spermatogonial stem cells and spermatogenesis in mice, monkeys and men[J]. Stem Cell Research, 2018, 29: 207-214. |
| 39 | DE ROOIJ D G. Proliferation and differentiation of spermatogonial stem cells[J]. Reproduction, 2001, 121(3): 347-354. |
| 40 | DYM M, KOKKINAKI M, HE Z P. Spermatogonial stem cells: mouse and human comparisons[J]. Birth Defects Research Part C, Embryo Today: Reviews, 2009, 87(1): 27-34. |
| 41 | MAHMOUD H. Concise review: spermatogenesis in an artificial three-dimensional system[J]. Stem Cells, 2012, 30(11): 2355-2360. |
| 42 | YOSHIDA S. Mouse spermatogenesis reflects the unity and diversity of tissue stem cell niche systems[J]. Cold Spring Harbor Perspectives in Biology, 2020, 12(12): a036186. |
| 43 | WEI B H, HAO S L, YANG W X. Regulation of spermatogonial stem cell self-renewal and proliferation in mammals[J]. Histology and Histopathology, 2022, 37(9): 825-838. |
| 44 | 余志鑫, 李鹏宇, 李凯, 等. 精原干细胞微环境研究进展[J]. 遗传, 2022, 44(12): 1103-1116. |
| YU Z X, LI P Y, LI K, et al. Progress on spermatogonial stem cell microenvironment[J]. Hereditas(Beijing), 2022, 44(12): 1103-1116. | |
| 45 | CHEN S R, LIU Y X. Regulation of spermatogonial stem cell self-renewal and spermatocyte meiosis by Sertoli cell signaling[J]. Reproduction, 2015, 149(4): R159-R167. |
| 46 | OATLEY J M, BRINSTER R L. Regulation of spermatogonial stem cell self-renewal in mammals[J]. Annual Review of Cell and Developmental Biology, 2008, 24: 263-286. |
| 47 | PELZMAN D L, ORWIG K E, HWANG K. Progress in translational reproductive science: testicular tissue transplantation and in vitro spermatogenesis[J]. Fertility and Sterility, 2020, 113(3): 500-509. |
| 48 | CHAMPY C. Quelques résultats de la méthode de culture des tissus[J]. Archives de Zoologie Expérimentale et Générale, 1920, 60: 461-500. |
| 49 | SATO T, KATAGIRI K, GOHBARA A, et al. In vitro production of functional sperm in cultured neonatal mouse testes[J]. Nature, 2011, 471(7339): 504-507. |
| 50 | SATO T, KATAGIRI K, KOJIMA K, et al. In vitro spermatogenesis in explanted adult mouse testis tissues[J]. PLoS One, 2015, 10(6): e0130171. |
| 51 | 郭雪江. 人类精子体外发生的研究展望[J]. 南京医科大学学报(自然科学版), 2021, 41(2): 157-159, 180. |
| GUO X J. Prospects of studies of human in vitro spermatogenesis[J]. Journal of Nanjing Medical University (Natural Sciences), 2021, 41(2): 157-159, 180. | |
| 52 | MOHAQIQ M, MOVAHEDIN M, MAZAHERI Z, et al. In vitro transplantation of spermatogonial stem cells isolated from human frozen-thawed testis tissue can induce spermatogenesis under 3-dimensional tissue culture conditions[J]. Biological Research, 2019, 52(1): 16. |
| 53 | YUAN Y, LI L H, CHENG Q, et al. In vitro testicular organogenesis from human fetal gonads produces fertilization-competent spermatids[J]. Cell Research, 2020, 30(3): 244-255. |
| 54 | SILVA A M D, PEREIRA A F, COMIZZOLI P, et al. Cryopreservation and culture of testicular tissues: an essential tool for biodiversity preservation[J]. Biopreservation and Biobanking, 2020, 18(3): 235-243. |
| 55 | BAERT Y, DE KOCK J, ALVES-LOPES J P, et al. Primary human testicular cells self-organize into organoids with testicular properties[J]. Stem Cell Reports, 2017, 8(1): 30-38. |
| 56 | CORTEZ J, LEIVA B, TORRES C G, et al. Generation and characterization of bovine testicular organoids derived from primary somatic cell populations[J]. Animals, 2022, 12(17): 2283. |
| 57 | XIE B, QIN Z, HUANG B, et al. In vitro culture and differentiation of buffalo (Bubalus bubalis) spermatogonia[J]. Reproduction in Domestic Animals, 2010, 45(2): 275-282. |
| 58 | WANG P, SUO L J, SHANG H, et al. Differentiation of spermatogonial stem cell-like cells from murine testicular tissue into haploid male germ cells in vitro [J]. Cytotechnology, 2014, 66(3): 365-372. |
| 59 | DANN C T, ALVARADO A L, MOLYNEUX L A, et al. Spermatogonial stem cell self-renewal requires OCT4, a factor downregulated during retinoic acid-induced differentiation[J]. Stem Cells, 2008, 26(11): 2928-2937. |
| 60 | CHO I K, EASLEY C A. Recent developments in in vitro spermatogenesis and future directions[J]. Reproductive Medicine, 2023, 4(3): 215-232. |
| 61 | SASAKI K, YOKOBAYASHI S, NAKAMURA T, et al. Robust in vitro induction of human germ cell fate from pluripotent stem cells[J]. Cell Stem Cell, 2015, 17(2): 178-194. |
| 62 | ZHOU Q, WANG M, YUAN Y, et al. Complete meiosis from embryonic stem cell-derived germ cells in vitro [J]. Cell Stem Cell, 2016, 18(3): 330-340. |
| 63 | BUCAY N, YEBRA M, CIRULLI V, et al. A novel approach for the derivation of putative primordial germ cells and sertoli cells from human embryonic stem cells[J]. Stem Cells, 2009, 27(1): 68-77. |
| 64 | YANG Y, SU Z J, XU W T, et al. Directed mouse embryonic stem cells into leydig-like cells rescue testosterone-deficient male rats in vivo [J]. Stem Cells and Development, 2015, 24(4): 459-470. |
| 65 | RODRÍGUEZ GUTIÉRREZ D, EID W, BIASON-LAUBER A. A human gonadal cell model from induced pluripotent stem cells[J]. Frontiers in Genetics, 2018, 9: 498. |
| 66 | ROBINSON M, WITHERSPOON L, WILLERTH S, et al. A novel organoid model of in vitro spermatogenesis using human induced pluripotent stem cells[EB/OL]. bioRxiv, 2021: 2021.06.04.447122[2023-11-01]. . |
| 67 | LI Z K, WANG L Y, WANG L B, et al. Generation of bimaternal and bipaternal mice from hypomethylated haploid ESCs with imprinting region deletions[J]. Cell Stem Cell, 2018, 23(5): 665-676.e4. |
| 68 | MURAKAMI K, HAMAZAKI N, HAMADA N, et al. Generation of functional oocytes from male mice in vitro [J]. Nature, 2023, 615(7954): 900-906. |
| 69 | ALVES-LOPES J P, STUKENBORG J B. Testicular organoids: a new model to study the testicular microenvironment in vitro?[J]. Human Reproduction Update, 2018, 24(2): 176-191. |
| 70 | YOKONISHI T, SATO T, KATAGIRI K, et al. In vitro reconstruction of mouse seminiferous tubules supporting germ cell differentiation[J]. Biology of Reproduction, 2013, 89(1): 15. |
| 71 | SALEM M, KHADIVI F, JAVANBAKHT P, et al. Advances of three-dimensional (3D) culture systems for in vitro spermatogenesis[J]. Stem Cell Research & Therapy, 2023, 14(1): 262. |
| 72 | REZAEI TOPRAGGALEH T, REZAZADEH VALOJERDI M, MONTAZERI L, et al. A testis-derived macroporous 3D scaffold as a platform for the generation of mouse testicular organoids[J]. Biomaterials Science, 2019, 7(4): 1422-1436. |
| 73 | RICHER G, HOBBS R M, LOVELAND K L, et al. Long-term maintenance and meiotic entry of early germ cells in murine testicular organoids functionalized by 3D printed scaffolds and air-medium interface cultivation[J]. Frontiers in Physiology, 2021, 12: 757565. |
| 74 | KANBAR M, VERMEULEN M, WYNS C. Organoids as tools to investigate the molecular mechanisms of male infertility and its treatments[J]. Reproduction, 2021, 161(5): R103-R112. |
| 75 | RICHER G, BAERT Y, GOOSSENS E. In-vitro spermatogenesis through testis modelling: toward the generation of testicular organoids[J]. Andrology, 2020, 8(4): 879-891. |
| 76 | SAKIB S, GOLDSMITH T, VOIGT A, et al. Testicular organoids to study cell-cell interactions in the mammalian testis[J]. Andrology, 2020, 8(4): 835-841. |
| 77 | BHANG D H, KIM B J, KIM B G, et al. Testicular endothelial cells are a critical population in the germline stem cell niche[J]. Nature Communications, 2018, 9(1): 4379. |
| 78 | DEFALCO T, POTTER S J, WILLIAMS A V, et al. Macrophages contribute to the spermatogonial niche in the adult testis[J]. Cell Reports, 2015, 12(7): 1107-1119. |
| 79 | MIURA C, KUWAHARA R, MIURA T. Transfer of spermatogenesis-related cDNAs into eel testis germ-somatic cell coculture pellets by electroporation: methods for analysis of gene function[J]. Molecular Reproduction and Development, 2007, 74(4): 420-427. |
| 80 | KANATSU-SHINOHARA M, INOUE K, TAKASHIMA S, et al. Reconstitution of mouse spermatogonial stem cell niches in culture[J]. Cell Stem Cell, 2012, 11(4): 567-578. |
| 81 | LI F P, YAMAGUCHI K, OKADA K, et al. Efficient transfection of DNA into primarily cultured rat Sertoli cells by electroporation[J]. Biology of Reproduction, 2013, 88(3): 61. |
| 82 | CONG L, RAN F A, COX D, et al. Multiplex genome engineering using CRISPR/Cas systems[J]. Science, 2013, 339(6121): 819-823. |
| 83 | GOLDSMITH T M, SAKIB S, WEBSTER D, et al. A reduction of primary cilia but not hedgehog signaling disrupts morphogenesis in testicular organoids[J]. Cell and Tissue Research, 2020, 380(1): 191-200. |
| 84 | LANCASTER M A, KNOBLICH J A. Organogenesis in a dish: modeling development and disease using organoid technologies[J]. Science, 2014, 345(6194): 1247125. |
| 85 | 李英奇, 李申宁, 朱海美, 等. 雄性生殖毒性的体外试验方法研究进展[J]. 中国新药杂志, 2021, 30(22): 2064-2068. |
| LI Y Q, LI S N, ZHU H M, et al. Advances in the methods of evaluating male reproductive toxicity in vitro [J]. Chinese Journal of New Drugs, 2021, 30(22): 2064-2068. | |
| 86 | ALVES-LOPES J P, SÖDER O, STUKENBORG J B. Testicular organoid generation by a novel in vitro three-layer gradient system[J]. Biomaterials, 2017, 130: 76-89. |
| 87 | CHENG C Y, MRUK D D. The blood-testis barrier and its implications for male contraception[J]. Pharmacological Reviews, 2012, 64(1): 16-64. |
| 88 | PENDERGRAFT S S, SADRI-ARDEKANI H, ATALA A, et al. Three-dimensional testicular organoid: a novel tool for the study of human spermatogenesis and gonadotoxicity in vitro [J]. Biology of Reproduction, 2017, 96(3): 720-732. |
| 89 | SAKIB S, UCHIDA A, VALENZUELA-LEON P, et al. Formation of organotypic testicular organoids in microwell culture[J]. Biology of Reproduction, 2019, 100(6): 1648-1660. |
| 90 | STRANGE D P, ZARANDI N P, TRIVEDI G, et al. Human testicular organoid system as a novel tool to study Zika virus pathogenesis[J]. Emerging Microbes & Infections, 2018, 7(1): 82. |
| 91 | YANG W, ZHANG C, WU Y H, et al. Mice 3D testicular organoid system as a novel tool to study Zika virus pathogenesis[J]. Virologica Sinica, 2023, 38(1): 66-74. |
| 92 | SAKIB S, LARA N L E M, HUYNH B C, et al. Organotypic rat testicular organoids for the study of testicular maturation and toxicology[J]. Frontiers in Endocrinology, 2022, 13: 892342. |
| 93 | ALBAMONTE M I, VITULLO A D. Preservation of fertility in female and male prepubertal patients diagnosed with cancer[J]. Journal of Assisted Reproduction and Genetics, 2023, 40(12): 2755-2767. |
| 94 | GOOSSENS E, JAHNUKAINEN K, MITCHELL R T, et al. Fertility preservation in boys: recent developments and new insights[J]. Human Reproduction Open, 2020, 2020(3): hoaa016. |
| 95 | YASMIN E, MITCHELL R, LANE S L. Preservation of fertility in teenagers and young adults treated for haematological malignancies[J]. The Lancet Haematology, 2021, 8(2): e149-e160. |
| 96 | LEVINE J, CANADA A, STERN C J. Fertility preservation in adolescents and young adults with cancer[J]. Journal of Clinical Oncology, 2010, 28(32): 4831-4841. |
| 97 | FAYOMI A P, PETERS K, SUKHWANI M, et al. Autologous grafting of cryopreserved prepubertal rhesus testis produces sperm and offspring[J]. Science, 2019, 363(6433): 1314-1319. |
| 98 | JENSEN J R, MORBECK D E, CODDINGTON C C 3rd. Fertility preservation[J]. Mayo Clinic Proceedings, 2011, 86(1): 45-49. |
| 99 | GIUDICE M G, DE MICHELE F, POELS J, et al. Update on fertility restoration from prepubertal spermatogonial stem cells: how far are we from clinical practice?[J]. Stem Cell Research, 2017, 21: 171-177. |
| 100 | DE MICHELE F, VERMEULEN M, WYNS C. Fertility restoration with spermatogonial stem cells[J]. Current Opinion in Endocrinology, Diabetes, and Obesity, 2017, 24(6): 424-431. |
| 101 | LARA N L E M, SAKIB S, DOBRINSKI I. Regulation of cell types within testicular organoids[J]. Endocrinology, 2021, 162(4): bqab033. |
| 102 | 程玮璐, 王泽华, 张译丹, 等. 类器官技术在医疗领域的应用和监管挑战[J]. 中国组织工程研究, 2025, 29(1): 202-210. |
| CHENG W L, WANG Z H, ZHANG Y D, et al. Application and regulatory challenges of organoid technology in medical field[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(1): 202-210. | |
| 103 | HANDELM A, EPPIGJ J, SCHIMENTIJ C. Applying “gold standards” to in-vitro-derived germ cells[J]. Cell, 2014, 157(6): 1257-1261. |
| [1] | 竺方欢, 岑雪聪, 陈振. 微生物合成二元醇研究进展[J]. 合成生物学, 2024, 5(6): 1367-1385. |
| [2] | 曹荣凯, 秦建华, 王亚清. 胎盘芯片及其在生殖医学领域的研究进展[J]. 合成生物学, 2024, 5(4): 831-850. |
| [3] | 黄利利, 张韩, 王伟伟, 谢海燕. 基于生物正交反应的病毒功能化及其生物医学应用[J]. 合成生物学, 2022, 3(2): 335-351. |
| [4] | 曾丹, 储建林, 陈燕茹, 范代娣. 人造蛋白功能材料的生物合成及应用[J]. 合成生物学, 2021, 2(4): 528-542. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||