合成生物学 ›› 2024, Vol. 5 ›› Issue (4): 851-866.DOI: 10.12211/2096-8280.2023-104
血管化类器官的构建方法及生物材料
李石开1,2, 曾东鳌1,2, 杜方舟2, 张京钟1,2, 余爽1,2
- 1.中国科学技术大学,生命科学与医学部,生物医学工程学院(苏州),安徽 合肥 230026
2.中国科学院苏州生物医学工程技术研究所,江苏 苏州 215163
-
收稿日期:2023-12-04修回日期:2024-02-29出版日期:2024-08-31发布日期:2024-09-19 -
通讯作者:张京钟,余爽 -
作者简介:李石开 (1997—),男,博士研究生。研究方向为干细胞结合生物材料在皮肤功能性重建中的应用。E-mail:lishikai26@163.com张京钟 (1973—),男,研究员,博士生导师。研究方向为干细胞/类脑器官治疗神经系统重大疾病,类器官芯片互联为微生理系统及其应用开发等。E-mail:zhangjz@sibet.ac.cn余爽 (1977—),女,研究员,博士生导师。研究方向为干细胞/类器官培养及相关的细胞替代疗法在皮肤功能性重建中的应用,干细胞/外泌体技术在神经精神疾病中的应用及其机制探索等。E-mail:yush@sibet.ac.cn -
基金资助:国家重点研发计划(2021YFA1101100);国家自然科学基金(82271522);姑苏重大创新团队项目(ZXT2019007)
The construction approaches and biomaterials for vascularized organoids
LI Shikai1,2, ZENG Dong′ao1,2, DU Fangzhou2, ZHANG Jingzhong1,2, YU Shuang1,2
- 1.School of Biomedical Engineering (Suzhou),Division of Life Science and Medicine,University of Science and Technology of China,Hefei 230026,Anhui,China
2.Suzhou Institute of Biomedical Engineering and Technology,Chinese Academy of Sciences,Suzhou 215163,Jiangsu,China
-
Received:2023-12-04Revised:2024-02-29Online:2024-08-31Published:2024-09-19 -
Contact:ZHANG Jingzhong, YU Shuang
摘要:
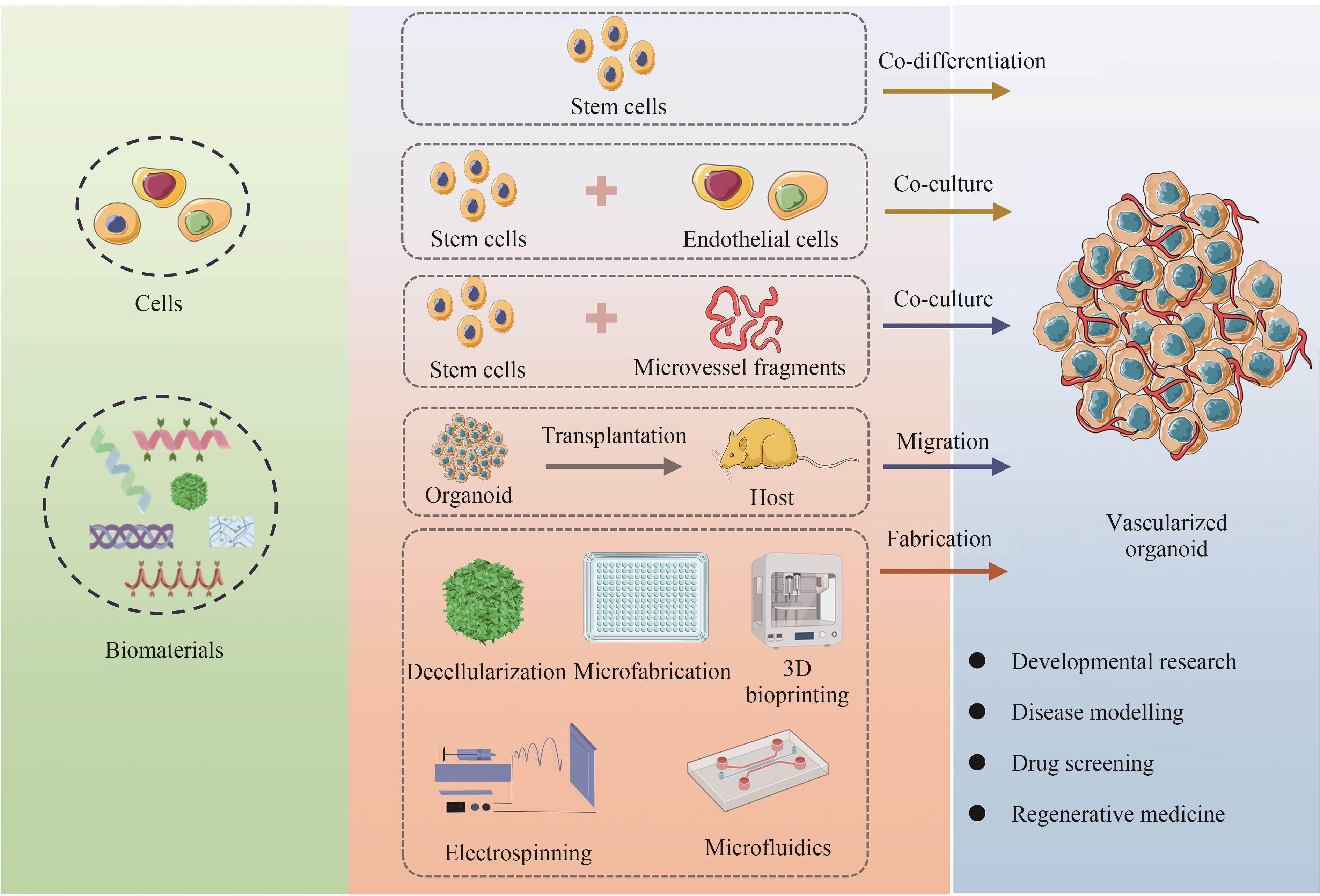
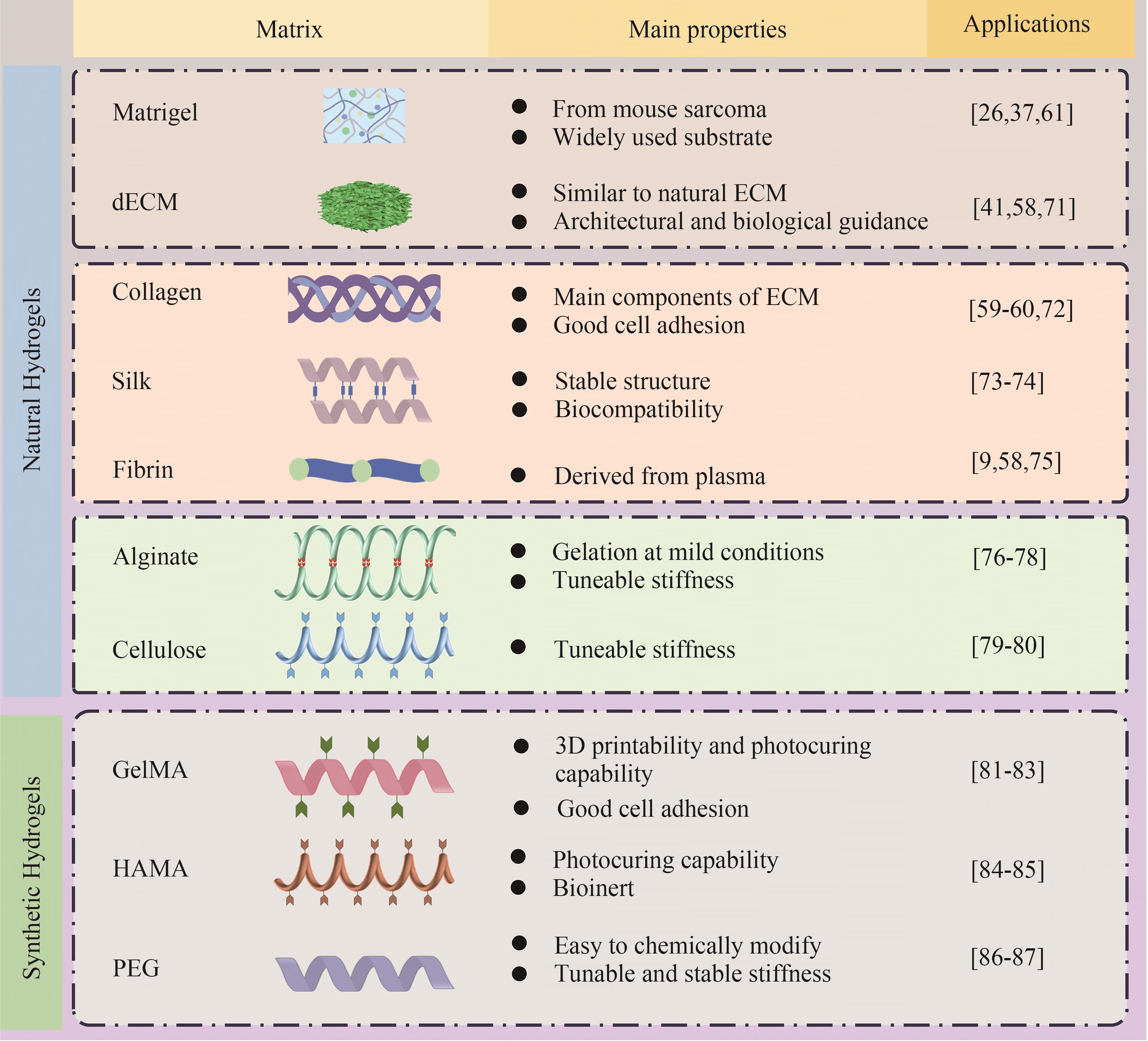
类器官血管化是完善类器官结构、功能及支持其体外长期存活的关键问题。近年来,随着类器官培养及生物工程技术的发展,类器官血管化有了长足的进步。本文综述了血管化类器官领域的最新进展,总结了目前用于血管化的构建策略与方法,包括干细胞共分化、多细胞共培养、微血管片段,移植后体内再血管化等生物技术,以及微制造、静电纺丝、三维生物打印、微流控技术等工程技术手段在血管化类器官方面的应用。血管化类器官的构建通常会辅以生物材料来负载血管化相关因子或提供不同类型细胞生长的微环境,本文对构建血管化类器官中应用的天然及合成生物材料也做了相应讨论。虽然类器官血管化目前还存在一定的局限性,但随着对血管化关键机制的解析及生物工程技术的进步,多种构建方法及生物材料的联合应用,将极大促进结构及功能完善的血管化类器官构建,并实质性地推动类器官技术在基础及临床医学领域的应用。
中图分类号:
引用本文
李石开, 曾东鳌, 杜方舟, 张京钟, 余爽. 血管化类器官的构建方法及生物材料[J]. 合成生物学, 2024, 5(4): 851-866.
LI Shikai, ZENG Dong′ao, DU Fangzhou, ZHANG Jingzhong, YU Shuang. The construction approaches and biomaterials for vascularized organoids[J]. Synthetic Biology Journal, 2024, 5(4): 851-866.
| 1 | JORGENSEN A M, YOO J J, ATALA A. Solid organ bioprinting: strategies to achieve organ function[J]. Chemical Reviews, 2020, 120(19): 11093-11127. |
| 2 | WOLF K J, WEISS J D, UZEL S G M, et al. Biomanufacturing human tissues via organ building blocks[J]. Cell Stem Cell, 2022, 29(5): 667-677. |
| 3 | LEE J, VAN DER VALK W H, SERDY S A, et al. Generation and characterization of hair-bearing skin organoids from human pluripotent stem cells[J]. Nature Protocols, 2022, 17(5): 1266-1305. |
| 4 | MA J, LIU J, GAO D Q, et al. Establishment of human pluripotent stem cell-derived skin organoids enabled pathophysiological model of SARS-CoV-2 infection[J]. Advanced Science, 2022, 9(7): e2104192. |
| 5 | HONG Z X, ZHU S T, LI H, et al. Bioengineered skin organoids: from development to applications[J]. Military Medical Research, 2023, 10(1): 40. |
| 6 | VARGAS-VALDERRAMA A, MESSINA A, MITJAVILA-GARCIA M T, et al. The endothelium, a key actor in organ development and hPSC-derived organoid vascularization[J]. Journal of Biomedical Science, 2020, 27(1): 67. |
| 7 | TANG X Y, WU S S, WANG D, et al. Human organoids in basic research and clinical applications[J]. Signal Transduction and Targeted Therapy, 2022, 7(1): 168. |
| 8 | RAFII S, BUTLER J M, DING B S. Angiocrine functions of organ-specific endothelial cells[J]. Nature, 2016, 529(7586): 316-325. |
| 9 | RAJASEKAR S, LIN D S Y, ABDUL L, et al. IFlowPlate-a customized 384-well plate for the culture of perfusable vascularized colon organoids[J]. Advanced Materials, 2020, 32(46): e2002974. |
| 10 | FU J Y, WANG D A. In situ organ-specific vascularization in tissue engineering[J]. Trends in Biotechnology, 2018, 36(8): 834-849. |
| 11 | SKARDAL A, SHUPE T, ATALA A. Organoid-on-a-chip and body-on-a-chip systems for drug screening and disease modeling[J]. Drug Discovery Today, 2016, 21(9): 1399-1411. |
| 12 | HAN R N N, POST M, TANSWELL A K, et al. Insulin-like growth factor-I receptor-mediated vasculogenesis/angiogenesis in human lung development[J]. American Journal of Respiratory Cell and Molecular Biology, 2003, 28(2): 159-169. |
| 13 | MISHRA A. Angiogenic neovessels promote tissue hypoxia[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(38): 10458-10460. |
| 14 | CHUNG A S, FERRARA N. Developmental and pathological angiogenesis[J]. Annual Review of Cell and Developmental Biology, 2011, 27: 563-584. |
| 15 | LEE H W, XU Y Y, HE L Q, et al. Role of venous endothelial cells in developmental and pathologic angiogenesis[J]. Circulation, 2021, 144(16): 1308-1322. |
| 16 | PÉREZ-GUTIÉRREZ L, FERRARA N. Biology and therapeutic targeting of vascular endothelial growth factor A[J]. Nature Reviews Molecular Cell Biology, 2023, 24(11): 816-834. |
| 17 | RODRIGUEZ RODIRGUEZ Y, MURPHY J, JEONG K, et al. FAK inhibition reduces hemangioma proliferation by blocking YAP mediated HBEGF expression[J]. Circulation Research, 2021, 129(): AP488. |
| 18 | LIU H T, ZHANG X, LIU J Y, et al. Vascularization of engineered organoids[J]. BMEMat, 2023, 1(3): e12031. |
| 19 | LOW J H, LI P, CHEW E G Y, et al. Generation of human PSC-derived kidney organoids with patterned nephron segments and a de novo vascular network[J]. Cell Stem Cell, 2019, 25(3): 373-387.e9. |
| 20 | SPENCE J R, MAYHEW C N, RANKIN S A, et al. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro [J]. Nature, 2011, 470(7332): 105-109. |
| 21 | HOLLOWAY E M, WU J H, CZERWINSKI M, et al. Differentiation of human intestinal organoids with endogenous vascular endothelial cells[J]. Developmental Cell, 2020, 54(4): 516-528.e7. |
| 22 | LEWIS-ISRAELI Y R, WASSERMAN A H, GABALSKI M A, et al. Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease[J]. Nature Communications, 2021, 12(1): 5142. |
| 23 | CUI K L, CHEN T W, ZHU Y J, et al. Engineering placenta-like organoids containing endogenous vascular cells from human-induced pluripotent stem cells[J]. Bioengineering & Translational Medicine, 2023, 8(1): e10390. |
| 24 | SHI Y C, SUN L, WANG M D, et al. Vascularized human cortical organoids (vOrganoids) model cortical development in vivo [J]. PLoS Biology, 2020, 18(5): e3000705. |
| 25 | WÖRSDÖRFER P, DALDA N, KERN A, et al. Generation of complex human organoid models including vascular networks by incorporation of mesodermal progenitor cells[J]. Scientific Reports, 2019, 9(1): 15663. |
| 26 | SUN X Y, JU X C, LI Y, et al. Generation of vascularized brain organoids to study neurovascular interactions[J]. eLife, 2022, 11: e76707. |
| 27 | SARASWATI S, MARROW S M W, WATCH L A, et al. Identification of a pro-angiogenic functional role for FSP1-positive fibroblast subtype in wound healing[J]. Nature Communications, 2019, 10(1): 3027. |
| 28 | NEWMAN A C, NAKATSU M N, CHOU W, et al. The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation[J]. Molecular Biology of the Cell, 2011, 22(20): 3791-3800. |
| 29 | STEVENS K R, KREUTZIGER K L, DUPRAS S K, et al. Physiological function and transplantation of scaffold-free and vascularized human cardiac muscle tissue[J]. Proceedings of the National Academy of Sciences of the United States of America, 2009, 106(39): 16568-16573. |
| 30 | MA J G, QIN C, WU J F, et al. 3D printing of strontium silicate microcylinder-containing multicellular biomaterial inks for vascularized skin regeneration[J]. Advanced Healthcare Materials, 2021, 10(16): e2100523. |
| 31 | STROBEL H A, LABELLE S A, KRISHNAN L, et al. Stromal cells promote neovascular invasion across tissue interfaces[J]. Frontiers in Physiology, 2020, 11: 1026. |
| 32 | STROBEL H A, GERTON T, HOYING J B. Vascularized adipocyte organoid model using isolated human microvessel fragments[J]. Biofabrication, 2021, 13(3): 035022. |
| 33 | SHEPHERD B R, CHEN H Y S, SMITH C M, et al. Rapid perfusion and network remodeling in a microvascular construct after implantation[J]. Arteriosclerosis, Thrombosis, and Vascular Biology, 2004, 24(5): 898-904. |
| 34 | QUAN Y P, ZHANG Y T, LI J, et al. Transplantation of in vitro prefabricated adipose organoids attenuates skin fibrosis by restoring subcutaneous fat and inducing dermal adipogenesis[J]. FASEB Journal, 2023, 37(8): e23076. |
| 35 | NALBACH L, ROMA L P, SCHMITT B M, et al. Improvement of islet transplantation by the fusion of islet cells with functional blood vessels[J]. EMBO Molecular Medicine, 2021, 13(1): e12616. |
| 36 | DYE B R, HILL D R, FERGUSON M A H, et al. In vitro generation of human pluripotent stem cell derived lung organoids[J]. eLife, 2015, 4: e05098. |
| 37 | MANSOUR A A, GONÇALVES J T, BLOYD C W, et al. Erratum: an in vivo model of functional and vascularized human brain organoids[J]. Nature Biotechnology, 2018, 36(5): 432-441. |
| 38 | WIMMER R A, LEOPOLDI A, AICHINGER M, et al. Human blood vessel organoids as a model of diabetic vasculopathy[J]. Nature, 2019, 565(7740): 505-510. |
| 39 | CORTEZ A R, POLING H M, BROWN N E, et al. Transplantation of human intestinal organoids into the mouse mesentery: a more physiologic and anatomic engraftment site[J]. Surgery, 2018, 164(4): 643-650. |
| 40 | WANG K, WANG X, HAN C S, et al. Scaffold-supported transplantation of islets in the epididymal fat pad of diabetic mice[J]. Journal of Visualized Experiments, 2017(125): e54995. |
| 41 | RAIKWAR S P, KIM E M, SIVITZ W I, et al. Human iPS cell-derived insulin producing cells form vascularized organoids under the kidney capsules of diabetic mice[J]. PLoS One, 2015, 10(1): e0116582. |
| 42 | LIM D, JACKSON J D, ATALA A, et al. Leading approaches to vascularize kidney constructs in tissue engineering[J]. Engineering, 2022, 19(12): 117-127. |
| 43 | ZHU L Y, YUHAN J Y, YU H, et al. Decellularized extracellular matrix for remodeling bioengineering organoid’s microenvironment[J]. Small, 2023, 19(25): e2207752. |
| 44 | KIM J W, NAM S A, YI J, et al. Kidney decellularized extracellular matrix enhanced the vascularization and maturation of human kidney organoids[J]. Advanced Science, 2022, 9(15): e2103526. |
| 45 | XU Z Y, HUANG J J, LIU Y, et al. Extracellular matrix bioink boosts stemness and facilitates transplantation of intestinal organoids as a biosafe Matrigel alternative[J]. Bioengineering & Translational Medicine, 2023, 8(1): e10327. |
| 46 | KITANO K, SCHWARTZ D M, ZHOU H Y, et al. Bioengineering of functional human induced pluripotent stem cell-derived intestinal grafts[J]. Nature Communications, 2017, 8(1): 765. |
| 47 | VELASCO V, SHARIATI S A, ESFANDYARPOUR R. Microtechnology-based methods for organoid models[J]. Microsystems & Nanoengineering, 2020, 6: 76. |
| 48 | WANG Y L, GUNASEKARA D B, REED M I, et al. A microengineered collagen scaffold for generating a polarized crypt-villus architecture of human small intestinal epithelium[J]. Biomaterials, 2017, 128: 44-55. |
| 49 | YANG K S, LEE J S, HAN S W, et al. Endothelial-neurosphere crosstalk in microwell arrays regulates self-renewal and differentiation of human neural stem cells[J]. Journal of Industrial and Engineering Chemistry, 2019, 74: 148-157. |
| 50 | LAI Benjamin F L, LU Rick X Z, HU Y S, et al. Recapitulating pancreatic tumor microenvironment through synergistic use of patient organoids and organ-on-a-chip vasculature[J]. Advanced Functional Materials, 2020, 30(48): 2000545. |
| 51 | TAKEBE T, SEKINE K, KIMURA M, et al. Massive and reproducible production of liver buds entirely from human pluripotent stem cells[J]. Cell Reports, 2017, 21(10): 2661-2670. |
| 52 | AL-DHAHEBI A M, LING J, KRISHNAN S G, et al. Electrospinning research and products: the road and the way forward[J]. Applied Physics Reviews, 2022, 9(1): 011319. |
| 53 | JAYASINGHE S N. Unspooling the history of cell electrospinning[J]. Matter, 2022, 5(1): 4-7. |
| 54 | RITZAU-REID K I, CALLENS S J P, XIE R X, et al. Microfibrous scaffolds guide stem cell lumenogenesis and brain organoid engineering[J]. Advanced Materials, 2023, 35(41): e2300305. |
| 55 | WANG C, LU W W, WANG M. Multifunctional fibrous scaffolds for bone regeneration with enhanced vascularization[J]. Journal of Materials Chemistry B, 2020, 8(4): 636-647. |
| 56 | GONG J, GONG Y, ZOU T, et al. A controllable perfusion microfluidic chip for facilitating the development of retinal ganglion cells in human retinal organoids[J]. Lab on a Chip, 2023, 23(17): 3820-3836. |
| 57 | MARCOS L F, WILSON S L, ROACH P. Tissue engineering of the retina: from organoids to microfluidic chips[J]. Journal of Tissue Engineering, 2021, 12: 20417314211059876. |
| 58 | HOMAN K A, GUPTA N, KROLL K T, et al. Flow-enhanced vascularization and maturation of kidney organoids in vitro [J]. Nature Methods, 2019, 16(3): 255-262. |
| 59 | BONANINI F, KUREK D, PREVIDI S, et al. In vitro grafting of hepatic spheroids and organoids on a microfluidic vascular bed[J]. Angiogenesis, 2022, 25(4): 455-470. |
| 60 | KOLESKY D B, HOMAN K A, SKYLAR-SCOTT M A, et al. Three-dimensional bioprinting of thick vascularized tissues[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(12): 3179-3184. |
| 61 | SALMON I, GREBENYUK S, FATTAH A R A, et al. Engineering neurovascular organoids with 3D printed microfluidic chips[J]. Lab on a Chip, 2022, 22(8): 1615-1629. |
| 62 | MIRONOV V, BOLAND T, TRUSK T, et al. Organ printing: computer-aided jet-based 3D tissue engineering[J]. Trends in Biotechnology, 2003, 21(4): 157-161. |
| 63 | PFISTER A, LANDERS R, LAIB A, et al. Biofunctional rapid prototyping for tissue-engineering applications: 3D bioplotting versus 3D printing[J]. Journal of Polymer Science Part A: Polymer Chemistry, 2004, 42(3): 624-638. |
| 64 | LI S K, LI Z H, YANG J, et al. Inhibition of sympathetic activation by delivering calcium channel blockers from a 3D printed scaffold to promote bone defect repair[J]. Advanced Healthcare Materials, 2022, 11(16): e2200785. |
| 65 | MA X Y, QU X, ZHU W, et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(8): 2206-2211. |
| 66 | YAP K K, GERRAND Y W, DINGLE A M, et al. Liver sinusoidal endothelial cells promote the differentiation and survival of mouse vascularised hepatobiliary organoids[J]. Biomaterials, 2020, 251: 120091. |
| 67 | TSENG T C, HSIEH F Y, THEATO P, et al. Glucose-sensitive self-healing hydrogel as sacrificial materials to fabricate vascularized constructs[J]. Biomaterials, 2017, 133: 20-28. |
| 68 | HOSSEINI M, KOEHLER K R, SHAFIEE A. Biofabrication of human skin with its appendages[J]. Advanced Healthcare Materials, 2022, 11(22): e2201626. |
| 69 | VEDADGHAVAMI A, MINOOEI F, MOHAMMADI M H, et al. Manufacturing of hydrogel biomaterials with controlled mechanical properties for tissue engineering applications[J]. Acta Biomaterialia, 2017, 62: 42-63. |
| 70 | LIU H T, WANG Y Q, CUI K L, et al. Advances in hydrogels in organoids and organs-on-a-chip[J]. Advanced Materials, 2019, 31(50): e1902042. |
| 71 | KIM J, KIM J, GAO G, et al. Bioprinted organoids platform with tumor vasculature for implementing precision personalized medicine targeted towards gastric cancer[J]. Advanced Functional Materials, 2023: 2306676. |
| 72 | MORGAN J P, DELNERO P F, ZHENG Y, et al. Formation of microvascular networks in vitro [J]. Nature Protocols, 2013, 8(9): 1820-1836. |
| 73 | GRAÇA M F P, MIGUEL S P, CABRAL C S D, et al. Hyaluronic acid-Based wound dressings: a review[J]. Carbohydrate Polymers, 2020, 241: 116364. |
| 74 | WRAY L S, TSIORIS K, GI E S, et al. Slowly degradable porous silk microfabricated scaffolds for vascularized tissue formation[J]. Advanced Functional Materials, 2013, 23(27): 3404-3412. |
| 75 | LUO L L, LIU L B, DING Y X, et al. Advances in biomimetic hydrogels for organoid culture[J]. Chemical Communications, 2023, 59(64): 9675-9686. |
| 76 | ZHANG Y S, PI Q M, VAN GENDEREN A M. Microfluidic bioprinting for engineering vascularized tissues and organoids[J]. Journal of Visualized Experiments, 2017(126): e55957. |
| 77 | HUANG J J, XU Z Y, JIAO J, et al. Microfluidic intestinal organoid-on-a-chip uncovers therapeutic targets by recapitulating oxygen dynamics of intestinal IR injury[J]. Bioactive Materials, 2023, 30: 1-14. |
| 78 | DALY A C, CUNNIFFE G M, SATHY B N, et al. 3D bioprinting of developmentally inspired templates for whole bone organ engineering[J]. Advanced Healthcare Materials, 2016, 5(18): 2353-2362. |
| 79 | WANG H, LIU H T, LIU H, et al. One-step generation of core-shell gelatin methacrylate (GelMA) microgels using a droplet microfluidic system[J]. Advanced Materials Technologies, 2019, 4(6): 1800632. |
| 80 | GUO L Q, LIANG Z H, YANG L, et al. The role of natural polymers in bone tissue engineering[J]. Journal of Controlled Release, 2021, 338: 571-582. |
| 81 | ZHU B W, WANG D Z, PAN H P, et al. Three-in-one customized bioink for islet organoid: GelMA/ECM/PRP orchestrate pro-angiogenic and immunoregulatory function[J]. Colloids and Surfaces B, Biointerfaces, 2023, 221: 113017. |
| 82 | ESCUDERO M, VAYSSE L, EKE G, et al. Scalable generation of pre-vascularized and functional human beige adipose organoids[J]. Advanced Science, 2023, 10(31): e2301499. |
| 83 | SADR N, ZHU M J, OSAKI T, et al. SAM-based cell transfer to photopatterned hydrogels for microengineering vascular-like structures[J]. Biomaterials, 2011, 32(30): 7479-7490. |
| 84 | WANG D Z, GUO Y B, ZHU J C, et al. Hyaluronic acid methacrylate/pancreatic extracellular matrix as a potential 3D printing bioink for constructing islet organoids[J]. Acta Biomaterialia, 2023, 165: 86-101. |
| 85 | EKE G, MANGIR N, HASIRCI N, et al. Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering[J]. Biomaterials, 2017, 129: 188-198. |
| 86 | BARRY C, SCHMITZ M T, PROPSON N E, et al. Uniform neural tissue models produced on synthetic hydrogels using standard culture techniques[J]. Experimental Biology and Medicine, 2017, 242(17): 1679-1689. |
| 87 | MILLER J S, STEVENS K R, YANG M T, et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues[J]. Nature Materials, 2012, 11(9): 768-774. |
| 88 | WANG X X, WANG X S, LIU J J, et al. Hair follicle and sebaceous gland de novo regeneration with cultured epidermal stem cells and skin-derived precursors[J]. Stem Cells Translational Medicine, 2016, 5(12): 1695-1706. |
| 89 | CHACÓN-MARTÍNEZ C A, KLOSE M, NIEMANN C, et al. Hair follicle stem cell cultures reveal self-organizing plasticity of stem cells and theirprogeny[J]. The EMBO Journal, 2017, 36(2): 151-164. |
| 90 | ZHANG X Y, XIAO S E, LIU B C, et al. Use of extracellular matrix hydrogel from human placenta to restore hair-inductive potential of dermal papilla cells[J]. Regenerative Medicine, 2019, 14(8): 741-751. |
| 91 | YAO B, WANG R, WANG Y H, et al. Biochemical and structural cues of 3D-printed matrix synergistically direct MSC differentiation for functional sweat gland regeneration[J]. Science Advances, 2020, 6(10): eaaz1094. |
| 92 | NANMO A, YAN L, ASABA T, et al. Bioprinting of hair follicle germs for hair regenerative medicine[J]. Acta Biomaterialia, 2023, 165: 50-59. |
| 93 | BROGUIERE N, ISENMANN L, HIRT C, et al. Growth of epithelial organoids in a defined hydrogel[J]. Advanced Materials, 2018, 30(43): e1801621. |
| 94 | SOZZI E, KAJTEZ J, BRUZELIUS A, et al. Silk scaffolding drives self-assembly of functional and mature human brain organoids[J]. Frontiers in Cell and Developmental Biology, 2022, 10: 1023279. |
| 95 | KALABUSHEVA E, TERSKIKH V, VOROTELYAK E. Hair germ model in vitro via human postnatal keratinocyte-dermal papilla interactions: impact of hyaluronic acid[J]. Stem Cells International, 2017, 2017: 9271869. |
| 96 | KAGEYAMA T, YOSHIMURA C, MYASNIKOVA D, et al. Spontaneous hair follicle germ (HFG) formation in vitro, enabling the large-scale production of HFGs for regenerative medicine[J]. Biomaterials, 2018, 154: 291-300. |
| 97 | WANG R, WANG Y H, YAO B, et al. Redirecting differentiation of mammary progenitor cells by 3D bioprinted sweat gland microenvironment[J]. Burns & Trauma, 2019, 7: 29. |
| 98 | KRÜGER M, OOSTERHOFF L A, VAN WOLFEREN M E, et al. Cellulose nanofibril hydrogel promotes hepatic differentiation of human liver organoids[J]. Advanced Healthcare Materials, 2020, 9(6): e1901658. |
| 99 | NIE J, GAO Q, WANG Y D, et al. Vessel-on-a-chip with hydrogel-based microfluidics[J]. Small, 2018, 14(45): e1802368. |
| 100 | TENG Y Y, ZOU M L, LIU S Y, et al. Dual-action icariin-containing thermosensitive hydrogel for wound macrophage polarization and hair-follicle Neogenesis [J]. Frontiers in Bioengineering and Biotechnology, 2022, 10: 902894. |
| 101 | LI H H, CHEN L, ZENG S P, et al. Matrigel basement membrane matrix induces eccrine sweat gland cells to reconstitute sweat gland-like structures in nude mice[J]. Experimental Cell Research, 2015, 332(1): 67-77. |
| 102 | KAGEYAMA T, SHIMIZU A, ANAKAMA R, et al. Reprogramming of three-dimensional microenvironments for in vitro hair follicle induction[J]. Science Advances, 2022, 8(42): eadd4603. |
| 103 | SHI W, MIRZA S, KUSS M, et al. Embedded bioprinting of breast tumor cells and organoids using low-concentration collagen-based bioinks[J]. Advanced Healthcare Materials, 2023, 12(26): e2300905. |
| 104 | YAMANLAR S, SANT S, BOUDOU T, et al. Surface functionalization of hyaluronic acid hydrogels by polyelectrolyte multilayer films[J]. Biomaterials, 2011, 32(24): 5590-5599. |
| 105 | JEON E Y, SORRELLS L, ABACI H E. Biomaterials and bioengineering to guide tissue morphogenesis in epithelial organoids[J]. Frontiers in Bioengineering and Biotechnology, 2022, 10: 1038277. |
| 106 | LUTOLF M P, HUBBELL J A. Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering[J]. Nature Biotechnology, 2005, 23(1): 47-55. |
| 107 | TIBBITT M W, ANSETH K S. Hydrogels as extracellular matrix mimics for 3D cell culture[J]. Biotechnology and Bioengineering, 2009, 103(4): 655-663. |
| 108 | BADYLAK S F. The extracellular matrix as a scaffold for tissue reconstruction[J]. Seminars in Cell & Developmental Biology, 2002, 13(5): 377-383. |
| 109 | LI Y H, HAN Y, WANG X Y, et al. Multifunctional hydrogels prepared by dual ion cross-linking for chronic wound healing[J]. ACS Applied Materials & Interfaces, 2017, 9(19): 16054-16062. |
| 110 | NGUYEN E H, DALY W T, LE N N T, et al. Versatile synthetic alternatives to Matrigel for vascular toxicity screening and stem cell expansion[J]. Nature Biomedical Engineering, 2017, 1: 0096. |
| 111 | HOSSEINI M, SHAFIEE A. Engineering bioactive scaffolds for skin regeneration[J]. Small, 2021, 17(41): e2101384. |
| 112 | CARMELIET P, JAIN R K. Molecular mechanisms and clinical applications of angiogenesis[J]. Nature, 2011, 473(7347): 298-307. |
| 113 | NOLAN D J, GINSBERG M, ISRAELY E, et al. Molecular signatures of tissue-specific microvascular endothelial cell heterogeneity in organ maintenance and regeneration[J]. Developmental Cell, 2013, 26(2): 204-219. |
| 114 | LI X R, CARMELIET P. Targeting angiogenic metabolism in disease[J]. Science, 2018, 359(6382): 1335-1336. |
| 115 | TEUWEN L A, DRAOUI N, DUBOIS C, et al. Endothelial cell metabolism: an update anno 2017[J]. Current Opinion in Hematology, 2017, 24(3): 240-247. |
| 116 | AUGUSTIN H G, KOH G Y. Organotypic vasculature: from descriptive heterogeneity to functional pathophysiology[J]. Science, 2017, 357(6353): eaal2379. |
| 117 | REITERER M, BRANCO C M. Endothelial cells and organ function: applications and implications of understanding unique and reciprocal remodelling[J]. The FEBS Journal, 2020, 287(6): 1088-1100. |
| 118 | TRIMM E, RED-HORSE K. Vascular endothelial cell development and diversity[J]. Nature Reviews Cardiology, 2023, 20(3): 197-210. |
| 119 | CHOW B W, GU C H. The molecular constituents of the blood-brain barrier[J]. Trends in Neurosciences, 2015, 38(10): 598-608. |
| 120 | ITKIN T, GUR-COHEN S, SPENCER J A, et al. Distinct bone marrow blood vessels differentially regulate haematopoiesis[J]. Nature, 2016, 532(7599): 323-328. |
| 121 | RAJABI M, MOUSA S A. The role of angiogenesis in cancer treatment[J]. Biomedicines, 2017, 5(2): 34. |
| 122 | ILIFF A J, XU X Z S. A mechanosensitive GPCR that detects the bloody force[J]. Cell, 2018, 173(3): 542-544. |
| 123 | DE BOCK K, GEORGIADOU M, SCHOORS S, et al. Role of PFKFB3-driven glycolysis in vessel sprouting[J]. Cell, 2013, 154(3): 651-663. |
| 124 | POTENTE M, CARMELIET P. The link between angiogenesis and endothelial metabolism[J]. Annual Review of Physiology, 2017, 79: 43-66. |
| 125 | YUAN L, XIE S F, BAI H R, et al. Reconstruction of dynamic mammary mini gland in vitro for normal physiology and oncogenesis[J]. Nature Methods, 2023, 20(12): 2021-2033. |
| 126 | CHEN Y W, HUANG S X, DE CARVALHO A L R T, et al. A three-dimensional model of human lung development and disease from pluripotent stem cells[J]. Nature Cell Biology, 2017, 19(5): 542-549. |
| 127 | CAPOWSKI E E, SAMIMI K, MAYERL S J, et al. Reproducibility and staging of 3D human retinal organoids across multiple pluripotent stem cell lines[J]. Development, 2019, 146(1): dev171686. |
| 128 | PHIPSON B, ER P X, COMBES A N, et al. Evaluation of variability in human kidney organoids[J]. Nature Methods, 2019, 16(1): 79-87. |
| [1] | 胡博文, 陈家斌, 刘晓东. 人类早期胚胎发育体外模型研究进展[J]. 合成生物学, 2024, 5(4): 719-733. |
| [2] | 蔡冰玉, 谭象天, 李伟. 合成生物学在干细胞工程化改造中的研究进展[J]. 合成生物学, 2024, 5(4): 782-794. |
| [3] | 张博航, 祁晓萱, 袁艳. 睾丸类器官在体外精子发生中的研究进展[J]. 合成生物学, 2024, 5(4): 770-781. |
| [4] | 韩宜钊, 郭佳, 邵玥. 干细胞模拟发育:细胞元件、胚胎模型与工程方法[J]. 合成生物学, 2024, 5(4): 734-753. |
| [5] | 胡可儿, 王汉奇, 黄儒麒, 张灿阳, 邢新会, 马少华. 整合设计策略下的工程化类器官与类器官芯片技术[J]. 合成生物学, 2024, 5(4): 883-897. |
| [6] | 陈子苓, 向阳飞. 类器官技术与合成生物学协同研究进展[J]. 合成生物学, 2024, 5(4): 795-812. |
| [7] | 艾宗勇, 张成庭, 牛宝华, 尹宇, 杨洁, 李天晴. 人胚胎早期发育与干细胞[J]. 合成生物学, 2024, 5(4): 700-718. |
| [8] | 陈倩文, 赵思琪, 彭耀进. 类器官:技术创新与伦理争议[J]. 合成生物学, 2024, 5(4): 898-907. |
| [9] | 洪源, 刘妍. 脑类器官在再生医学中的研究进展[J]. 合成生物学, 2024, 5(4): 754-769. |
| [10] | 曹荣凯, 秦建华, 王亚清. 胎盘芯片及其在生殖医学领域的研究进展[J]. 合成生物学, 2024, 5(4): 831-850. |
| [11] | 陈汐玥, 王亚清, 包芳, 秦建华. 肝器官芯片在生物医学研究中的应用进展[J]. 合成生物学, 2024, 5(4): 813-830. |
| [12] | 孟倩, 尹聪, 黄卫人. 肿瘤类器官及其在合成生物学中的研究进展[J]. 合成生物学, 2024, 5(1): 191-201. |
| [13] | 朱骊宇, 赵玉龙, 李伟, 王立宾. 哺乳动物染色体工程研究进展[J]. 合成生物学, 2023, 4(2): 394-406. |
| [14] | 朱润涛, 钟超, 戴卓君. 细菌生物被膜的软物质特性及其工程化应用[J]. 合成生物学, 2022, 3(4): 626-637. |
| [15] | 杨兆颖, 张帆, 郭建文, 高卫平. 类弹性蛋白多肽的生物合成及其药物递送应用[J]. 合成生物学, 2022, 3(4): 728-747. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||