Synthetic Biology Journal ›› 2024, Vol. 5 ›› Issue (4): 770-781.DOI: 10.12211/2096-8280.2023-095
• Invited Review • Previous Articles Next Articles
Advancements in testicular organoids for in vitro spermatogenesis
ZHANG Bohang, QI Xiaoxuan, YUAN Yan
- State Key Laboratory of Reproductive Medicine and Offspring Health,Nanjing Medical University,Nanjing 211166,Jiangsu,China
-
Received:2023-11-30Revised:2024-03-05Online:2024-09-19Published:2024-08-31 -
Contact:YUAN Yan
睾丸类器官在体外精子发生中的研究进展
张博航, 祁晓萱, 袁艳
- 南京医科大学生殖医学与子代健康全国重点实验室,江苏 南京 211166
-
通讯作者:袁艳 -
作者简介:张博航 (1999—),男,博士研究生。研究方向为精子发生过程中相关机制。E-mail:zhangbohang2018@163.com袁艳 (1987—),女,博士,教授,博士生导师。研究方向为体外男性生育力重构,包括胚胎干细胞(ESC)和诱导多能干细胞(iPSC)分化、睾丸类器官重构及相关机制。E-mail:yuanyan@njmu.edu.cn -
基金资助:国家重点研发计划(2022YFC2702800);国家自然科学基金(82122025)
CLC Number:
Cite this article
ZHANG Bohang, QI Xiaoxuan, YUAN Yan. Advancements in testicular organoids for in vitro spermatogenesis[J]. Synthetic Biology Journal, 2024, 5(4): 770-781.
张博航, 祁晓萱, 袁艳. 睾丸类器官在体外精子发生中的研究进展[J]. 合成生物学, 2024, 5(4): 770-781.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://synbioj.cip.com.cn/EN/10.12211/2096-8280.2023-095
| 1 | GRISWOLD M D. Spermatogenesis: the commitment to meiosis[J]. Physiological Reviews, 2016, 96(1): 1-17. |
| 2 | DU L, CHEN W, CHENG Z X, et al. Novel gene regulation in normal and abnormal spermatogenesis[J]. Cells, 2021, 10(3): 666. |
| 3 | OKONOFUA F E, NTOIMO L F C, OMONKHUA A, et al. Causes and risk factors for male infertility: a scoping review of published studies[J]. International Journal of General Medicine, 2022, 15: 5985-5997. |
| 4 | AGARWAL A, BASKARAN S, PAREKH N, et al. Male infertility[J]. Lancet, 2021, 397(10271): 319-333. |
| 5 | INHORN M C, PATRIZIO P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century[J]. Human Reproduction Update, 2015, 21(4): 411-426. |
| 6 | NJAGI P, GROOT W, ARSENIJEVIC J, et al. Financial costs of assisted reproductive technology for patients in low- and middle-income countries: a systematic review[J]. Human Reproduction Open, 2023, 2023(2): hoad007. |
| 7 | MCLACHLAN R I. Approach to the patient with oligozoospermia[J]. The Journal of Clinical Endocrinology and Metabolism, 2013, 98(3): 873-880. |
| 8 | SHAHROKHI S Z, SALEHI P, ALYASIN A, et al. Asthenozoospermia: cellular and molecular contributing factors and treatment strategies[J]. Andrologia, 2020, 52(2): e13463. |
| 9 | WOSNITZER M, GOLDSTEIN M, HARDY M P. Review of azoospermia[J]. Spermatogenesis, 2014, 4: e28218. |
| 10 | Practice Committee of the American Society for Reproductive Medicine in Collaboration with the Society for Male Reproduction and Urology. The management of obstructive azoospermia: a committee opinion[J]. Fertility and Sterility, 2019, 111(5): 873-880. |
| 11 | PICTON H M, WYNS C, ANDERSON R A, et al. A European perspective on testicular tissue cryopreservation for fertility preservation in prepubertal and adolescent boys[J]. Human Reproduction, 2015, 30(11): 2463-2475. |
| 12 | ALIAKBARI F, TAGHIZABET N, AZIZI F, et al. A review of methods for preserving male fertility[J]. Zygote, 2022, 30(3): 289-297. |
| 13 | HEZAVEHEI M, SHARAFI M, KOUCHESFAHANI H M, et al. Sperm cryopreservation: a review on current molecular cryobiology and advanced approaches[J]. Reproductive Biomedicine Online, 2018, 37(3): 327-339. |
| 14 | FATEHULLAH A, TAN S H, BARKER N. Organoids as an in vitro model of human development and disease[J]. Nature Cell Biology, 2016, 18(3): 246-254. |
| 15 | MCCAULEY H A, WELLS J M. Pluripotent stem cell-derived organoids: using principles of developmental biology to grow human tissues in a dish[J]. Development, 2017, 144(6): 958-962. |
| 16 | 李娟娟, 张君涛, 赵英博, 等. 类器官的研究进展及应用前景[J]. 中国畜牧兽医, 2021, 48(6): 1985-1994. |
| LI J J, ZHANG J T, ZHAO Y B, et al. Research progress and application prospect of organoids[J]. China Animal Husbandry & Veterinary Medicine, 2021, 48(6): 1985-1994. | |
| 17 | QUADRATO G, NGUYEN T, MACOSKO E Z, et al. Cell diversity and network dynamics in photosensitive human brain organoids[J]. Nature, 2017, 545(7652): 48-53. |
| 18 | TAKEBE T, SEKINE K, ENOMURA M, et al. Vascularized and functional human liver from an iPSC-derived organ bud transplant[J]. Nature, 2013, 499(7459): 481-484. |
| 19 | TAKEBE T, ZHANG R R, KOIKE H, et al. Generation of a vascularized and functional human liver from an iPSC-derived organ bud transplant[J]. Nature Protocols, 2014, 9(2): 396-409. |
| 20 | SCHMIDT C, DEYETT A, ILMER T, et al. Multi-chamber cardioids unravel human heart development and cardiac defects[J]. Cell, 2023, 186(25): 5587-5605.e27. |
| 21 | BOJ S F, HWANG C I, BAKER L A, et al. Organoid models of human and mouse ductal pancreatic cancer[J]. Cell, 2015, 160(1/2): 324-338. |
| 22 | MORGAN J P, DELNERO P F, ZHENG Y, et al. Formation of microvascular networks in vitro [J]. Nature Protocols, 2013, 8(9): 1820-1836. |
| 23 | WANG N Z, SHEN J M, MINGHUA L I U, et al. A brief history of testicular organoids: from theory to the wards[J]. Journal of Assisted Reproduction and Genetics, 2022, 39(7): 1423-1431. |
| 24 | 张栋, 杜黎, 何祖平. 男性生殖系统类器官的研究进展[J]. 湖南师范大学学报(医学版), 2022, 19(4): 1-6. |
| ZHANG D, DU L, HE Z P. Research advancement on the organoids of male reproductive system[J]. Journal of Hunan Normal University (Medical Sciences), 2022, 19(4): 1-6. | |
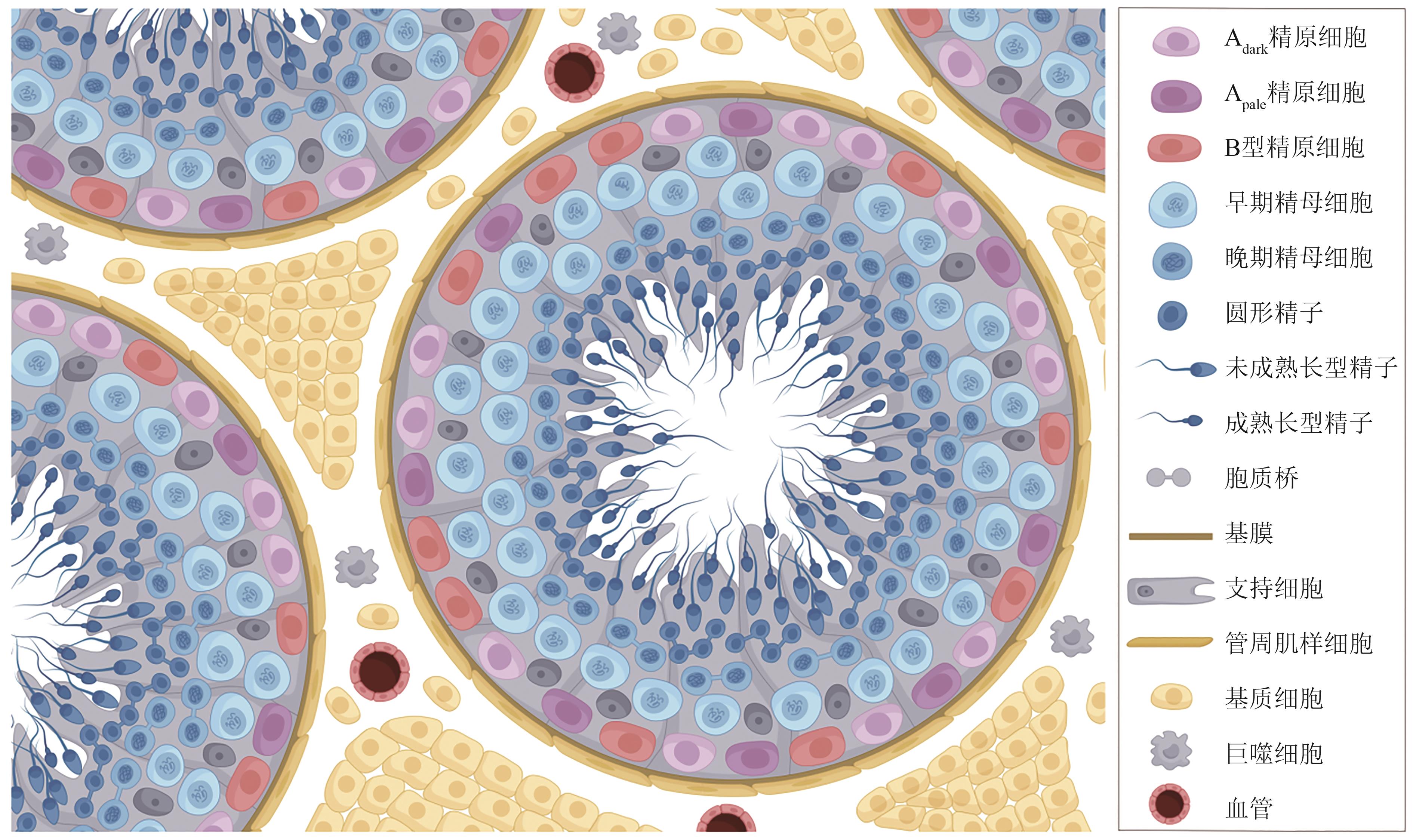
| 25 | SVINGEN T, KOOPMAN P. Building the mammalian testis: origins, differentiation, and assembly of the component cell populations[J]. Genes & Development, 2013, 27(22): 2409-2426. |
| 26 | MÄKELÄ J A, KOSKENNIEMI J J, VIRTANEN H E, et al. Testis development[J]. Endocrine Reviews, 2019, 40(4): 857-905. |
| 27 | 朱文倩, 蔡宁宁, 杨蕊, 等. 精子发生研究进展[J]. 生命科学, 2020, 32(10): 1021-1028. |
| ZHU W Q, CAI N N, YANG R, et al. Advances in spermatogenesis[J]. Chinese Bulletin of Life Sciences, 2020, 32(10): 1021-1028. | |
| 28 | GRISWOLD M D. The central role of Sertoli cells in spermatogenesis[J]. Seminars in Cell & Developmental Biology, 1998, 9(4): 411-416. |
| 29 | LUACES J P, TORO-URREGO N, OTERO-LOSADA M, et al. What do we know about blood-testis barrier? Current understanding of its structure and physiology[J]. Frontiers in Cell and Developmental Biology, 2023, 11: 1114769. |
| 30 | CHEN L Y, BROWN P R, WILLIS W B, et al. Peritubular myoid cells participate in male mouse spermatogonial stem cell maintenance[J]. Endocrinology, 2014, 155(12): 4964-4974. |
| 31 | MAEKAWA M, KAMIMURA K, NAGANO T. Peritubular myoid cells in the testis: their structure and function[J]. Archives of Histology and Cytology, 1996, 59(1): 1-13. |
| 32 | ZIRKIN B R, PAPADOPOULOS V. Leydig cells: formation, function, and regulation[J]. Biology of Reproduction, 2018, 99(1): 101-111 |
| 33 | MEINHARDT A, WANG M, SCHULZ C, et al. Microenvironmental signals govern the cellular identity of testicular macrophages[J]. Journal of Leukocyte Biology, 2018, 104(4): 757-766. |
| 34 | TAN K, SONG H W, WILKINSON M F. Single-cell RNAseq analysis of testicular germ and somatic cell development during the perinatal period[J]. Development, 2020, 147(3): dev183251. |
| 35 | O’DONNELL L, SMITH L B, REBOURCET D. Sertoli cells as key drivers of testis function[J]. Seminars in Cell & Developmental Biology, 2022, 121: 2-9. |
| 36 | ROBINSON M, SPARANESE S, WITHERSPOON L, et al. Human in vitro spermatogenesis as a regenerative therapy—where do we stand?[J]. Nature Reviews Urology, 2023, 20(8): 461-479. |
| 37 | MCLAREN A. Primordial germ cells in the mouse[J]. Developmental Biology, 2003, 262(1): 1-15. |
| 38 | FAYOMI A P, ORWIG K E. Spermatogonial stem cells and spermatogenesis in mice, monkeys and men[J]. Stem Cell Research, 2018, 29: 207-214. |
| 39 | DE ROOIJ D G. Proliferation and differentiation of spermatogonial stem cells[J]. Reproduction, 2001, 121(3): 347-354. |
| 40 | DYM M, KOKKINAKI M, HE Z P. Spermatogonial stem cells: mouse and human comparisons[J]. Birth Defects Research Part C, Embryo Today: Reviews, 2009, 87(1): 27-34. |
| 41 | MAHMOUD H. Concise review: spermatogenesis in an artificial three-dimensional system[J]. Stem Cells, 2012, 30(11): 2355-2360. |
| 42 | YOSHIDA S. Mouse spermatogenesis reflects the unity and diversity of tissue stem cell niche systems[J]. Cold Spring Harbor Perspectives in Biology, 2020, 12(12): a036186. |
| 43 | WEI B H, HAO S L, YANG W X. Regulation of spermatogonial stem cell self-renewal and proliferation in mammals[J]. Histology and Histopathology, 2022, 37(9): 825-838. |
| 44 | 余志鑫, 李鹏宇, 李凯, 等. 精原干细胞微环境研究进展[J]. 遗传, 2022, 44(12): 1103-1116. |
| YU Z X, LI P Y, LI K, et al. Progress on spermatogonial stem cell microenvironment[J]. Hereditas(Beijing), 2022, 44(12): 1103-1116. | |
| 45 | CHEN S R, LIU Y X. Regulation of spermatogonial stem cell self-renewal and spermatocyte meiosis by Sertoli cell signaling[J]. Reproduction, 2015, 149(4): R159-R167. |
| 46 | OATLEY J M, BRINSTER R L. Regulation of spermatogonial stem cell self-renewal in mammals[J]. Annual Review of Cell and Developmental Biology, 2008, 24: 263-286. |
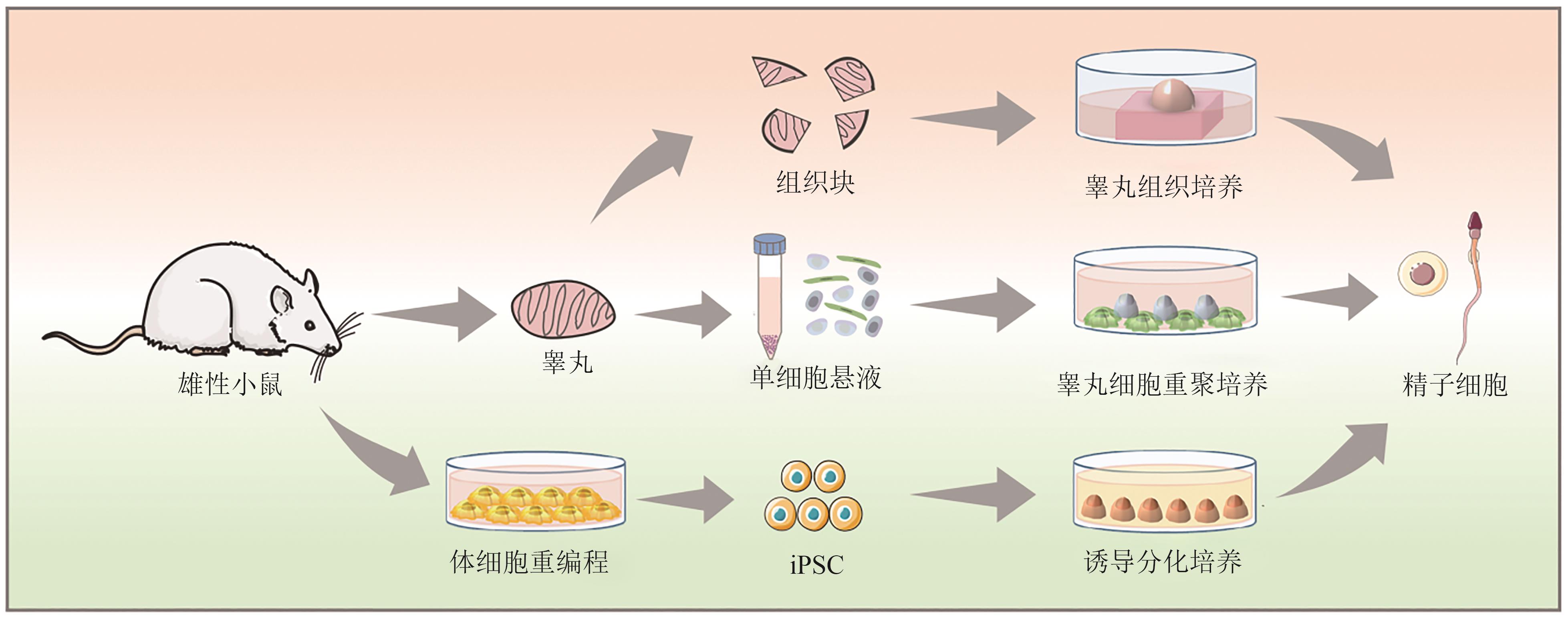
| 47 | PELZMAN D L, ORWIG K E, HWANG K. Progress in translational reproductive science: testicular tissue transplantation and in vitro spermatogenesis[J]. Fertility and Sterility, 2020, 113(3): 500-509. |
| 48 | CHAMPY C. Quelques résultats de la méthode de culture des tissus[J]. Archives de Zoologie Expérimentale et Générale, 1920, 60: 461-500. |
| 49 | SATO T, KATAGIRI K, GOHBARA A, et al. In vitro production of functional sperm in cultured neonatal mouse testes[J]. Nature, 2011, 471(7339): 504-507. |
| 50 | SATO T, KATAGIRI K, KOJIMA K, et al. In vitro spermatogenesis in explanted adult mouse testis tissues[J]. PLoS One, 2015, 10(6): e0130171. |
| 51 | 郭雪江. 人类精子体外发生的研究展望[J]. 南京医科大学学报(自然科学版), 2021, 41(2): 157-159, 180. |
| GUO X J. Prospects of studies of human in vitro spermatogenesis[J]. Journal of Nanjing Medical University (Natural Sciences), 2021, 41(2): 157-159, 180. | |
| 52 | MOHAQIQ M, MOVAHEDIN M, MAZAHERI Z, et al. In vitro transplantation of spermatogonial stem cells isolated from human frozen-thawed testis tissue can induce spermatogenesis under 3-dimensional tissue culture conditions[J]. Biological Research, 2019, 52(1): 16. |
| 53 | YUAN Y, LI L H, CHENG Q, et al. In vitro testicular organogenesis from human fetal gonads produces fertilization-competent spermatids[J]. Cell Research, 2020, 30(3): 244-255. |
| 54 | SILVA A M D, PEREIRA A F, COMIZZOLI P, et al. Cryopreservation and culture of testicular tissues: an essential tool for biodiversity preservation[J]. Biopreservation and Biobanking, 2020, 18(3): 235-243. |
| 55 | BAERT Y, DE KOCK J, ALVES-LOPES J P, et al. Primary human testicular cells self-organize into organoids with testicular properties[J]. Stem Cell Reports, 2017, 8(1): 30-38. |
| 56 | CORTEZ J, LEIVA B, TORRES C G, et al. Generation and characterization of bovine testicular organoids derived from primary somatic cell populations[J]. Animals, 2022, 12(17): 2283. |
| 57 | XIE B, QIN Z, HUANG B, et al. In vitro culture and differentiation of buffalo (Bubalus bubalis) spermatogonia[J]. Reproduction in Domestic Animals, 2010, 45(2): 275-282. |
| 58 | WANG P, SUO L J, SHANG H, et al. Differentiation of spermatogonial stem cell-like cells from murine testicular tissue into haploid male germ cells in vitro [J]. Cytotechnology, 2014, 66(3): 365-372. |
| 59 | DANN C T, ALVARADO A L, MOLYNEUX L A, et al. Spermatogonial stem cell self-renewal requires OCT4, a factor downregulated during retinoic acid-induced differentiation[J]. Stem Cells, 2008, 26(11): 2928-2937. |
| 60 | CHO I K, EASLEY C A. Recent developments in in vitro spermatogenesis and future directions[J]. Reproductive Medicine, 2023, 4(3): 215-232. |
| 61 | SASAKI K, YOKOBAYASHI S, NAKAMURA T, et al. Robust in vitro induction of human germ cell fate from pluripotent stem cells[J]. Cell Stem Cell, 2015, 17(2): 178-194. |
| 62 | ZHOU Q, WANG M, YUAN Y, et al. Complete meiosis from embryonic stem cell-derived germ cells in vitro [J]. Cell Stem Cell, 2016, 18(3): 330-340. |
| 63 | BUCAY N, YEBRA M, CIRULLI V, et al. A novel approach for the derivation of putative primordial germ cells and sertoli cells from human embryonic stem cells[J]. Stem Cells, 2009, 27(1): 68-77. |
| 64 | YANG Y, SU Z J, XU W T, et al. Directed mouse embryonic stem cells into leydig-like cells rescue testosterone-deficient male rats in vivo [J]. Stem Cells and Development, 2015, 24(4): 459-470. |
| 65 | RODRÍGUEZ GUTIÉRREZ D, EID W, BIASON-LAUBER A. A human gonadal cell model from induced pluripotent stem cells[J]. Frontiers in Genetics, 2018, 9: 498. |
| 66 | ROBINSON M, WITHERSPOON L, WILLERTH S, et al. A novel organoid model of in vitro spermatogenesis using human induced pluripotent stem cells[EB/OL]. bioRxiv, 2021: 2021.06.04.447122[2023-11-01]. . |
| 67 | LI Z K, WANG L Y, WANG L B, et al. Generation of bimaternal and bipaternal mice from hypomethylated haploid ESCs with imprinting region deletions[J]. Cell Stem Cell, 2018, 23(5): 665-676.e4. |
| 68 | MURAKAMI K, HAMAZAKI N, HAMADA N, et al. Generation of functional oocytes from male mice in vitro [J]. Nature, 2023, 615(7954): 900-906. |
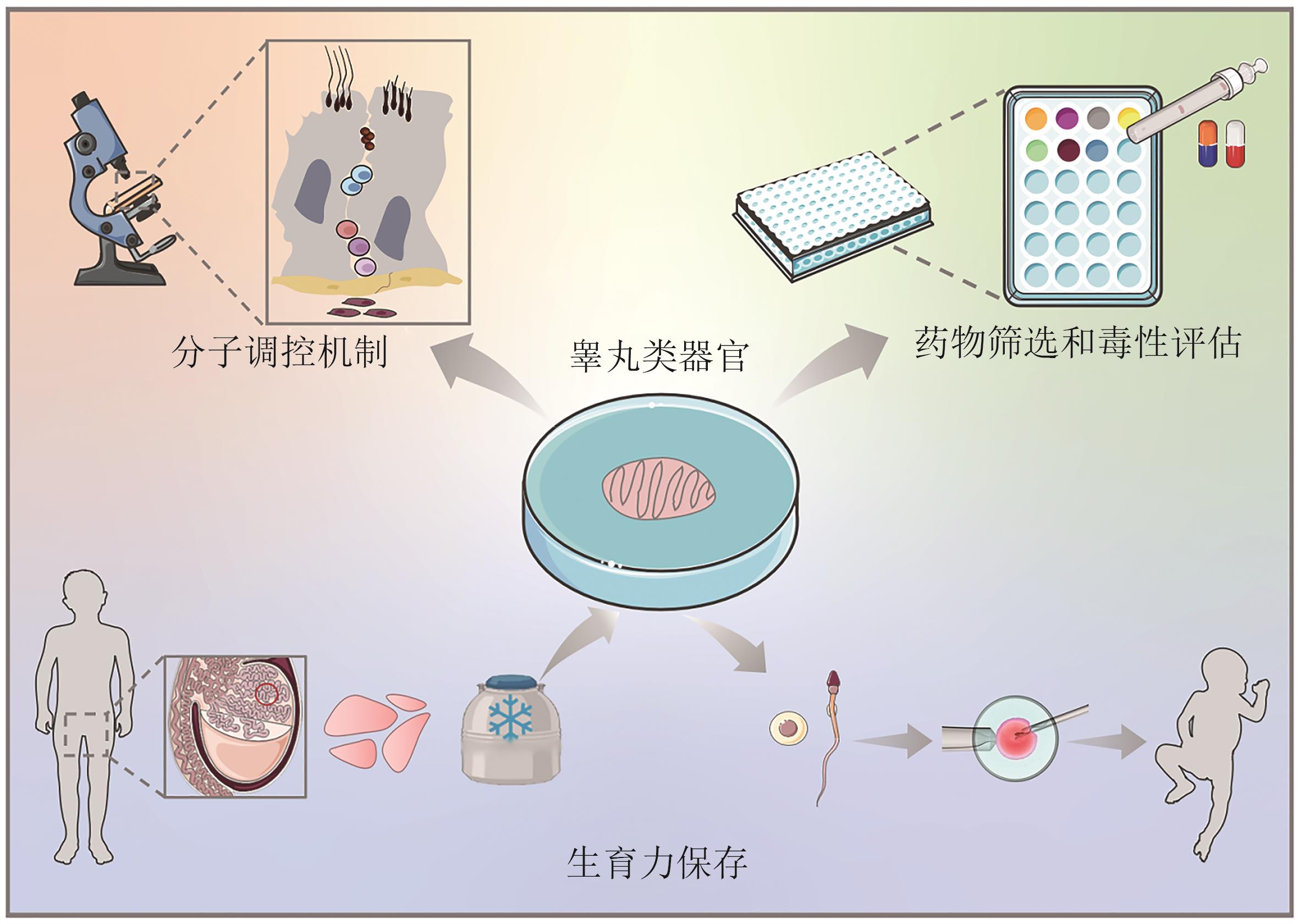
| 69 | ALVES-LOPES J P, STUKENBORG J B. Testicular organoids: a new model to study the testicular microenvironment in vitro?[J]. Human Reproduction Update, 2018, 24(2): 176-191. |
| 70 | YOKONISHI T, SATO T, KATAGIRI K, et al. In vitro reconstruction of mouse seminiferous tubules supporting germ cell differentiation[J]. Biology of Reproduction, 2013, 89(1): 15. |
| 71 | SALEM M, KHADIVI F, JAVANBAKHT P, et al. Advances of three-dimensional (3D) culture systems for in vitro spermatogenesis[J]. Stem Cell Research & Therapy, 2023, 14(1): 262. |
| 72 | REZAEI TOPRAGGALEH T, REZAZADEH VALOJERDI M, MONTAZERI L, et al. A testis-derived macroporous 3D scaffold as a platform for the generation of mouse testicular organoids[J]. Biomaterials Science, 2019, 7(4): 1422-1436. |
| 73 | RICHER G, HOBBS R M, LOVELAND K L, et al. Long-term maintenance and meiotic entry of early germ cells in murine testicular organoids functionalized by 3D printed scaffolds and air-medium interface cultivation[J]. Frontiers in Physiology, 2021, 12: 757565. |
| 74 | KANBAR M, VERMEULEN M, WYNS C. Organoids as tools to investigate the molecular mechanisms of male infertility and its treatments[J]. Reproduction, 2021, 161(5): R103-R112. |
| 75 | RICHER G, BAERT Y, GOOSSENS E. In-vitro spermatogenesis through testis modelling: toward the generation of testicular organoids[J]. Andrology, 2020, 8(4): 879-891. |
| 76 | SAKIB S, GOLDSMITH T, VOIGT A, et al. Testicular organoids to study cell-cell interactions in the mammalian testis[J]. Andrology, 2020, 8(4): 835-841. |
| 77 | BHANG D H, KIM B J, KIM B G, et al. Testicular endothelial cells are a critical population in the germline stem cell niche[J]. Nature Communications, 2018, 9(1): 4379. |
| 78 | DEFALCO T, POTTER S J, WILLIAMS A V, et al. Macrophages contribute to the spermatogonial niche in the adult testis[J]. Cell Reports, 2015, 12(7): 1107-1119. |
| 79 | MIURA C, KUWAHARA R, MIURA T. Transfer of spermatogenesis-related cDNAs into eel testis germ-somatic cell coculture pellets by electroporation: methods for analysis of gene function[J]. Molecular Reproduction and Development, 2007, 74(4): 420-427. |
| 80 | KANATSU-SHINOHARA M, INOUE K, TAKASHIMA S, et al. Reconstitution of mouse spermatogonial stem cell niches in culture[J]. Cell Stem Cell, 2012, 11(4): 567-578. |
| 81 | LI F P, YAMAGUCHI K, OKADA K, et al. Efficient transfection of DNA into primarily cultured rat Sertoli cells by electroporation[J]. Biology of Reproduction, 2013, 88(3): 61. |
| 82 | CONG L, RAN F A, COX D, et al. Multiplex genome engineering using CRISPR/Cas systems[J]. Science, 2013, 339(6121): 819-823. |
| 83 | GOLDSMITH T M, SAKIB S, WEBSTER D, et al. A reduction of primary cilia but not hedgehog signaling disrupts morphogenesis in testicular organoids[J]. Cell and Tissue Research, 2020, 380(1): 191-200. |
| 84 | LANCASTER M A, KNOBLICH J A. Organogenesis in a dish: modeling development and disease using organoid technologies[J]. Science, 2014, 345(6194): 1247125. |
| 85 | 李英奇, 李申宁, 朱海美, 等. 雄性生殖毒性的体外试验方法研究进展[J]. 中国新药杂志, 2021, 30(22): 2064-2068. |
| LI Y Q, LI S N, ZHU H M, et al. Advances in the methods of evaluating male reproductive toxicity in vitro [J]. Chinese Journal of New Drugs, 2021, 30(22): 2064-2068. | |
| 86 | ALVES-LOPES J P, SÖDER O, STUKENBORG J B. Testicular organoid generation by a novel in vitro three-layer gradient system[J]. Biomaterials, 2017, 130: 76-89. |
| 87 | CHENG C Y, MRUK D D. The blood-testis barrier and its implications for male contraception[J]. Pharmacological Reviews, 2012, 64(1): 16-64. |
| 88 | PENDERGRAFT S S, SADRI-ARDEKANI H, ATALA A, et al. Three-dimensional testicular organoid: a novel tool for the study of human spermatogenesis and gonadotoxicity in vitro [J]. Biology of Reproduction, 2017, 96(3): 720-732. |
| 89 | SAKIB S, UCHIDA A, VALENZUELA-LEON P, et al. Formation of organotypic testicular organoids in microwell culture[J]. Biology of Reproduction, 2019, 100(6): 1648-1660. |
| 90 | STRANGE D P, ZARANDI N P, TRIVEDI G, et al. Human testicular organoid system as a novel tool to study Zika virus pathogenesis[J]. Emerging Microbes & Infections, 2018, 7(1): 82. |
| 91 | YANG W, ZHANG C, WU Y H, et al. Mice 3D testicular organoid system as a novel tool to study Zika virus pathogenesis[J]. Virologica Sinica, 2023, 38(1): 66-74. |
| 92 | SAKIB S, LARA N L E M, HUYNH B C, et al. Organotypic rat testicular organoids for the study of testicular maturation and toxicology[J]. Frontiers in Endocrinology, 2022, 13: 892342. |
| 93 | ALBAMONTE M I, VITULLO A D. Preservation of fertility in female and male prepubertal patients diagnosed with cancer[J]. Journal of Assisted Reproduction and Genetics, 2023, 40(12): 2755-2767. |
| 94 | GOOSSENS E, JAHNUKAINEN K, MITCHELL R T, et al. Fertility preservation in boys: recent developments and new insights[J]. Human Reproduction Open, 2020, 2020(3): hoaa016. |
| 95 | YASMIN E, MITCHELL R, LANE S L. Preservation of fertility in teenagers and young adults treated for haematological malignancies[J]. The Lancet Haematology, 2021, 8(2): e149-e160. |
| 96 | LEVINE J, CANADA A, STERN C J. Fertility preservation in adolescents and young adults with cancer[J]. Journal of Clinical Oncology, 2010, 28(32): 4831-4841. |
| 97 | FAYOMI A P, PETERS K, SUKHWANI M, et al. Autologous grafting of cryopreserved prepubertal rhesus testis produces sperm and offspring[J]. Science, 2019, 363(6433): 1314-1319. |
| 98 | JENSEN J R, MORBECK D E, CODDINGTON C C 3rd. Fertility preservation[J]. Mayo Clinic Proceedings, 2011, 86(1): 45-49. |
| 99 | GIUDICE M G, DE MICHELE F, POELS J, et al. Update on fertility restoration from prepubertal spermatogonial stem cells: how far are we from clinical practice?[J]. Stem Cell Research, 2017, 21: 171-177. |
| 100 | DE MICHELE F, VERMEULEN M, WYNS C. Fertility restoration with spermatogonial stem cells[J]. Current Opinion in Endocrinology, Diabetes, and Obesity, 2017, 24(6): 424-431. |
| 101 | LARA N L E M, SAKIB S, DOBRINSKI I. Regulation of cell types within testicular organoids[J]. Endocrinology, 2021, 162(4): bqab033. |
| 102 | 程玮璐, 王泽华, 张译丹, 等. 类器官技术在医疗领域的应用和监管挑战[J]. 中国组织工程研究, 2025, 29(1): 202-210. |
| CHENG W L, WANG Z H, ZHANG Y D, et al. Application and regulatory challenges of organoid technology in medical field[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(1): 202-210. | |
| 103 | HANDELM A, EPPIGJ J, SCHIMENTIJ C. Applying “gold standards” to in-vitro-derived germ cells[J]. Cell, 2014, 157(6): 1257-1261. |
| [1] | ZHU Fanghuan, CEN Xuecong, CHEN Zhen. Research progress of diols production by microbes [J]. Synthetic Biology Journal, 2024, 5(6): 1367-1385. |
| [2] | Rongkai CAO, Jianhua QIN, Yaqing WANG. Advances in placenta-on-a-chip for reproductive medicine research [J]. Synthetic Biology Journal, 2024, 5(4): 831-850. |
| [3] | Lili HUANG, Han ZHANG, Weiwei WANG, Haiyan XIE. Bioorthogonal functionalization of viruses for biomedical applications [J]. Synthetic Biology Journal, 2022, 3(2): 335-351. |
| [4] | Dan ZENG, Jianlin CHU, Yanru CHEN, Daidi FAN. Biological synthesis and applications of artificial protein functional materials [J]. Synthetic Biology Journal, 2021, 2(4): 528-542. |
| [5] | Quansheng DU, Wei HONG, Yan ZU. Grant and funding for synthetic biology at NSFC from 2010 to 2019 [J]. Synthetic Biology Journal, 2020, 1(3): 385-394. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||