Synthetic Biology Journal ›› 2024, Vol. 5 ›› Issue (4): 851-866.DOI: 10.12211/2096-8280.2023-104
• Invited Review • Previous Articles Next Articles
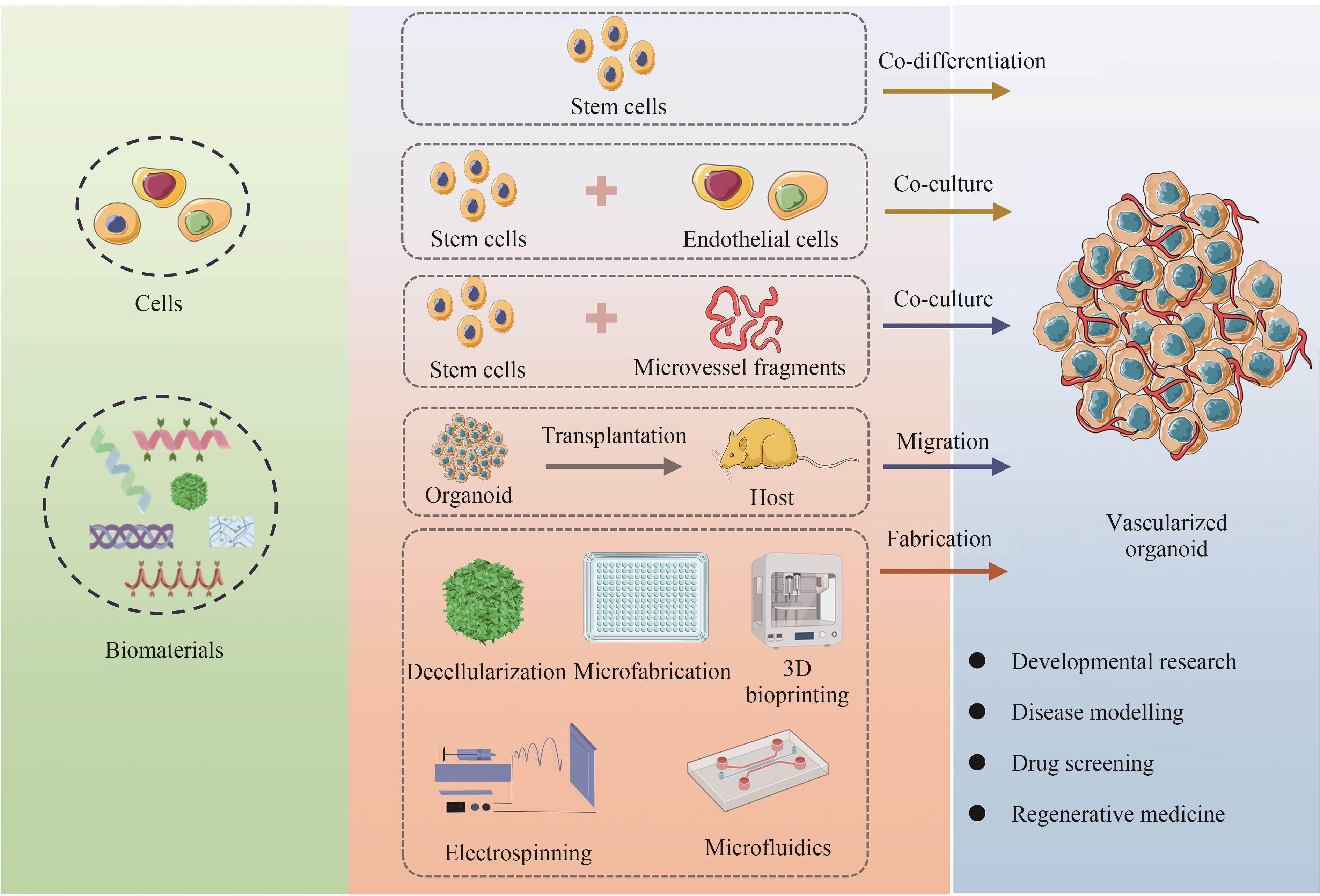
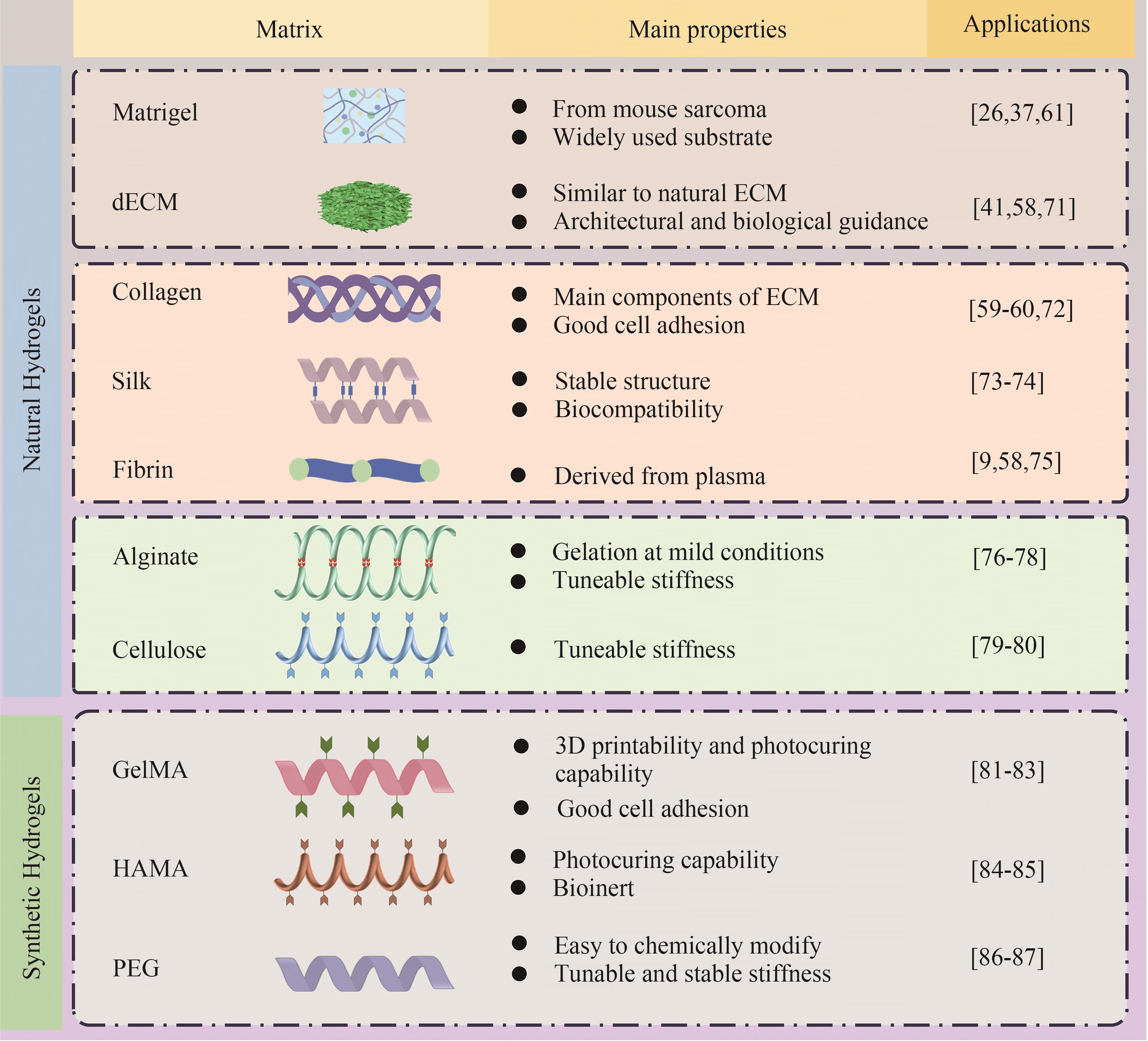
The construction approaches and biomaterials for vascularized organoids
LI Shikai1,2, ZENG Dong′ao1,2, DU Fangzhou2, ZHANG Jingzhong1,2, YU Shuang1,2
- 1.School of Biomedical Engineering (Suzhou),Division of Life Science and Medicine,University of Science and Technology of China,Hefei 230026,Anhui,China
2.Suzhou Institute of Biomedical Engineering and Technology,Chinese Academy of Sciences,Suzhou 215163,Jiangsu,China
-
Received:2023-12-04Revised:2024-02-29Online:2024-09-19Published:2024-08-31 -
Contact:ZHANG Jingzhong, YU Shuang
血管化类器官的构建方法及生物材料
李石开1,2, 曾东鳌1,2, 杜方舟2, 张京钟1,2, 余爽1,2
- 1.中国科学技术大学,生命科学与医学部,生物医学工程学院(苏州),安徽 合肥 230026
2.中国科学院苏州生物医学工程技术研究所,江苏 苏州 215163
-
通讯作者:张京钟,余爽 -
作者简介:李石开 (1997—),男,博士研究生。研究方向为干细胞结合生物材料在皮肤功能性重建中的应用。E-mail:lishikai26@163.com张京钟 (1973—),男,研究员,博士生导师。研究方向为干细胞/类脑器官治疗神经系统重大疾病,类器官芯片互联为微生理系统及其应用开发等。E-mail:zhangjz@sibet.ac.cn余爽 (1977—),女,研究员,博士生导师。研究方向为干细胞/类器官培养及相关的细胞替代疗法在皮肤功能性重建中的应用,干细胞/外泌体技术在神经精神疾病中的应用及其机制探索等。E-mail:yush@sibet.ac.cn -
基金资助:国家重点研发计划(2021YFA1101100);国家自然科学基金(82271522);姑苏重大创新团队项目(ZXT2019007)
CLC Number:
Cite this article
LI Shikai, ZENG Dong′ao, DU Fangzhou, ZHANG Jingzhong, YU Shuang. The construction approaches and biomaterials for vascularized organoids[J]. Synthetic Biology Journal, 2024, 5(4): 851-866.
李石开, 曾东鳌, 杜方舟, 张京钟, 余爽. 血管化类器官的构建方法及生物材料[J]. 合成生物学, 2024, 5(4): 851-866.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://synbioj.cip.com.cn/EN/10.12211/2096-8280.2023-104
| 1 | JORGENSEN A M, YOO J J, ATALA A. Solid organ bioprinting: strategies to achieve organ function[J]. Chemical Reviews, 2020, 120(19): 11093-11127. |
| 2 | WOLF K J, WEISS J D, UZEL S G M, et al. Biomanufacturing human tissues via organ building blocks[J]. Cell Stem Cell, 2022, 29(5): 667-677. |
| 3 | LEE J, VAN DER VALK W H, SERDY S A, et al. Generation and characterization of hair-bearing skin organoids from human pluripotent stem cells[J]. Nature Protocols, 2022, 17(5): 1266-1305. |
| 4 | MA J, LIU J, GAO D Q, et al. Establishment of human pluripotent stem cell-derived skin organoids enabled pathophysiological model of SARS-CoV-2 infection[J]. Advanced Science, 2022, 9(7): e2104192. |
| 5 | HONG Z X, ZHU S T, LI H, et al. Bioengineered skin organoids: from development to applications[J]. Military Medical Research, 2023, 10(1): 40. |
| 6 | VARGAS-VALDERRAMA A, MESSINA A, MITJAVILA-GARCIA M T, et al. The endothelium, a key actor in organ development and hPSC-derived organoid vascularization[J]. Journal of Biomedical Science, 2020, 27(1): 67. |
| 7 | TANG X Y, WU S S, WANG D, et al. Human organoids in basic research and clinical applications[J]. Signal Transduction and Targeted Therapy, 2022, 7(1): 168. |
| 8 | RAFII S, BUTLER J M, DING B S. Angiocrine functions of organ-specific endothelial cells[J]. Nature, 2016, 529(7586): 316-325. |
| 9 | RAJASEKAR S, LIN D S Y, ABDUL L, et al. IFlowPlate-a customized 384-well plate for the culture of perfusable vascularized colon organoids[J]. Advanced Materials, 2020, 32(46): e2002974. |
| 10 | FU J Y, WANG D A. In situ organ-specific vascularization in tissue engineering[J]. Trends in Biotechnology, 2018, 36(8): 834-849. |
| 11 | SKARDAL A, SHUPE T, ATALA A. Organoid-on-a-chip and body-on-a-chip systems for drug screening and disease modeling[J]. Drug Discovery Today, 2016, 21(9): 1399-1411. |
| 12 | HAN R N N, POST M, TANSWELL A K, et al. Insulin-like growth factor-I receptor-mediated vasculogenesis/angiogenesis in human lung development[J]. American Journal of Respiratory Cell and Molecular Biology, 2003, 28(2): 159-169. |
| 13 | MISHRA A. Angiogenic neovessels promote tissue hypoxia[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(38): 10458-10460. |
| 14 | CHUNG A S, FERRARA N. Developmental and pathological angiogenesis[J]. Annual Review of Cell and Developmental Biology, 2011, 27: 563-584. |
| 15 | LEE H W, XU Y Y, HE L Q, et al. Role of venous endothelial cells in developmental and pathologic angiogenesis[J]. Circulation, 2021, 144(16): 1308-1322. |
| 16 | PÉREZ-GUTIÉRREZ L, FERRARA N. Biology and therapeutic targeting of vascular endothelial growth factor A[J]. Nature Reviews Molecular Cell Biology, 2023, 24(11): 816-834. |
| 17 | RODRIGUEZ RODIRGUEZ Y, MURPHY J, JEONG K, et al. FAK inhibition reduces hemangioma proliferation by blocking YAP mediated HBEGF expression[J]. Circulation Research, 2021, 129(): AP488. |
| 18 | LIU H T, ZHANG X, LIU J Y, et al. Vascularization of engineered organoids[J]. BMEMat, 2023, 1(3): e12031. |
| 19 | LOW J H, LI P, CHEW E G Y, et al. Generation of human PSC-derived kidney organoids with patterned nephron segments and a de novo vascular network[J]. Cell Stem Cell, 2019, 25(3): 373-387.e9. |
| 20 | SPENCE J R, MAYHEW C N, RANKIN S A, et al. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro [J]. Nature, 2011, 470(7332): 105-109. |
| 21 | HOLLOWAY E M, WU J H, CZERWINSKI M, et al. Differentiation of human intestinal organoids with endogenous vascular endothelial cells[J]. Developmental Cell, 2020, 54(4): 516-528.e7. |
| 22 | LEWIS-ISRAELI Y R, WASSERMAN A H, GABALSKI M A, et al. Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease[J]. Nature Communications, 2021, 12(1): 5142. |
| 23 | CUI K L, CHEN T W, ZHU Y J, et al. Engineering placenta-like organoids containing endogenous vascular cells from human-induced pluripotent stem cells[J]. Bioengineering & Translational Medicine, 2023, 8(1): e10390. |
| 24 | SHI Y C, SUN L, WANG M D, et al. Vascularized human cortical organoids (vOrganoids) model cortical development in vivo [J]. PLoS Biology, 2020, 18(5): e3000705. |
| 25 | WÖRSDÖRFER P, DALDA N, KERN A, et al. Generation of complex human organoid models including vascular networks by incorporation of mesodermal progenitor cells[J]. Scientific Reports, 2019, 9(1): 15663. |
| 26 | SUN X Y, JU X C, LI Y, et al. Generation of vascularized brain organoids to study neurovascular interactions[J]. eLife, 2022, 11: e76707. |
| 27 | SARASWATI S, MARROW S M W, WATCH L A, et al. Identification of a pro-angiogenic functional role for FSP1-positive fibroblast subtype in wound healing[J]. Nature Communications, 2019, 10(1): 3027. |
| 28 | NEWMAN A C, NAKATSU M N, CHOU W, et al. The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation[J]. Molecular Biology of the Cell, 2011, 22(20): 3791-3800. |
| 29 | STEVENS K R, KREUTZIGER K L, DUPRAS S K, et al. Physiological function and transplantation of scaffold-free and vascularized human cardiac muscle tissue[J]. Proceedings of the National Academy of Sciences of the United States of America, 2009, 106(39): 16568-16573. |
| 30 | MA J G, QIN C, WU J F, et al. 3D printing of strontium silicate microcylinder-containing multicellular biomaterial inks for vascularized skin regeneration[J]. Advanced Healthcare Materials, 2021, 10(16): e2100523. |
| 31 | STROBEL H A, LABELLE S A, KRISHNAN L, et al. Stromal cells promote neovascular invasion across tissue interfaces[J]. Frontiers in Physiology, 2020, 11: 1026. |
| 32 | STROBEL H A, GERTON T, HOYING J B. Vascularized adipocyte organoid model using isolated human microvessel fragments[J]. Biofabrication, 2021, 13(3): 035022. |
| 33 | SHEPHERD B R, CHEN H Y S, SMITH C M, et al. Rapid perfusion and network remodeling in a microvascular construct after implantation[J]. Arteriosclerosis, Thrombosis, and Vascular Biology, 2004, 24(5): 898-904. |
| 34 | QUAN Y P, ZHANG Y T, LI J, et al. Transplantation of in vitro prefabricated adipose organoids attenuates skin fibrosis by restoring subcutaneous fat and inducing dermal adipogenesis[J]. FASEB Journal, 2023, 37(8): e23076. |
| 35 | NALBACH L, ROMA L P, SCHMITT B M, et al. Improvement of islet transplantation by the fusion of islet cells with functional blood vessels[J]. EMBO Molecular Medicine, 2021, 13(1): e12616. |
| 36 | DYE B R, HILL D R, FERGUSON M A H, et al. In vitro generation of human pluripotent stem cell derived lung organoids[J]. eLife, 2015, 4: e05098. |
| 37 | MANSOUR A A, GONÇALVES J T, BLOYD C W, et al. Erratum: an in vivo model of functional and vascularized human brain organoids[J]. Nature Biotechnology, 2018, 36(5): 432-441. |
| 38 | WIMMER R A, LEOPOLDI A, AICHINGER M, et al. Human blood vessel organoids as a model of diabetic vasculopathy[J]. Nature, 2019, 565(7740): 505-510. |
| 39 | CORTEZ A R, POLING H M, BROWN N E, et al. Transplantation of human intestinal organoids into the mouse mesentery: a more physiologic and anatomic engraftment site[J]. Surgery, 2018, 164(4): 643-650. |
| 40 | WANG K, WANG X, HAN C S, et al. Scaffold-supported transplantation of islets in the epididymal fat pad of diabetic mice[J]. Journal of Visualized Experiments, 2017(125): e54995. |
| 41 | RAIKWAR S P, KIM E M, SIVITZ W I, et al. Human iPS cell-derived insulin producing cells form vascularized organoids under the kidney capsules of diabetic mice[J]. PLoS One, 2015, 10(1): e0116582. |
| 42 | LIM D, JACKSON J D, ATALA A, et al. Leading approaches to vascularize kidney constructs in tissue engineering[J]. Engineering, 2022, 19(12): 117-127. |
| 43 | ZHU L Y, YUHAN J Y, YU H, et al. Decellularized extracellular matrix for remodeling bioengineering organoid’s microenvironment[J]. Small, 2023, 19(25): e2207752. |
| 44 | KIM J W, NAM S A, YI J, et al. Kidney decellularized extracellular matrix enhanced the vascularization and maturation of human kidney organoids[J]. Advanced Science, 2022, 9(15): e2103526. |
| 45 | XU Z Y, HUANG J J, LIU Y, et al. Extracellular matrix bioink boosts stemness and facilitates transplantation of intestinal organoids as a biosafe Matrigel alternative[J]. Bioengineering & Translational Medicine, 2023, 8(1): e10327. |
| 46 | KITANO K, SCHWARTZ D M, ZHOU H Y, et al. Bioengineering of functional human induced pluripotent stem cell-derived intestinal grafts[J]. Nature Communications, 2017, 8(1): 765. |
| 47 | VELASCO V, SHARIATI S A, ESFANDYARPOUR R. Microtechnology-based methods for organoid models[J]. Microsystems & Nanoengineering, 2020, 6: 76. |
| 48 | WANG Y L, GUNASEKARA D B, REED M I, et al. A microengineered collagen scaffold for generating a polarized crypt-villus architecture of human small intestinal epithelium[J]. Biomaterials, 2017, 128: 44-55. |
| 49 | YANG K S, LEE J S, HAN S W, et al. Endothelial-neurosphere crosstalk in microwell arrays regulates self-renewal and differentiation of human neural stem cells[J]. Journal of Industrial and Engineering Chemistry, 2019, 74: 148-157. |
| 50 | LAI Benjamin F L, LU Rick X Z, HU Y S, et al. Recapitulating pancreatic tumor microenvironment through synergistic use of patient organoids and organ-on-a-chip vasculature[J]. Advanced Functional Materials, 2020, 30(48): 2000545. |
| 51 | TAKEBE T, SEKINE K, KIMURA M, et al. Massive and reproducible production of liver buds entirely from human pluripotent stem cells[J]. Cell Reports, 2017, 21(10): 2661-2670. |
| 52 | AL-DHAHEBI A M, LING J, KRISHNAN S G, et al. Electrospinning research and products: the road and the way forward[J]. Applied Physics Reviews, 2022, 9(1): 011319. |
| 53 | JAYASINGHE S N. Unspooling the history of cell electrospinning[J]. Matter, 2022, 5(1): 4-7. |
| 54 | RITZAU-REID K I, CALLENS S J P, XIE R X, et al. Microfibrous scaffolds guide stem cell lumenogenesis and brain organoid engineering[J]. Advanced Materials, 2023, 35(41): e2300305. |
| 55 | WANG C, LU W W, WANG M. Multifunctional fibrous scaffolds for bone regeneration with enhanced vascularization[J]. Journal of Materials Chemistry B, 2020, 8(4): 636-647. |
| 56 | GONG J, GONG Y, ZOU T, et al. A controllable perfusion microfluidic chip for facilitating the development of retinal ganglion cells in human retinal organoids[J]. Lab on a Chip, 2023, 23(17): 3820-3836. |
| 57 | MARCOS L F, WILSON S L, ROACH P. Tissue engineering of the retina: from organoids to microfluidic chips[J]. Journal of Tissue Engineering, 2021, 12: 20417314211059876. |
| 58 | HOMAN K A, GUPTA N, KROLL K T, et al. Flow-enhanced vascularization and maturation of kidney organoids in vitro [J]. Nature Methods, 2019, 16(3): 255-262. |
| 59 | BONANINI F, KUREK D, PREVIDI S, et al. In vitro grafting of hepatic spheroids and organoids on a microfluidic vascular bed[J]. Angiogenesis, 2022, 25(4): 455-470. |
| 60 | KOLESKY D B, HOMAN K A, SKYLAR-SCOTT M A, et al. Three-dimensional bioprinting of thick vascularized tissues[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(12): 3179-3184. |
| 61 | SALMON I, GREBENYUK S, FATTAH A R A, et al. Engineering neurovascular organoids with 3D printed microfluidic chips[J]. Lab on a Chip, 2022, 22(8): 1615-1629. |
| 62 | MIRONOV V, BOLAND T, TRUSK T, et al. Organ printing: computer-aided jet-based 3D tissue engineering[J]. Trends in Biotechnology, 2003, 21(4): 157-161. |
| 63 | PFISTER A, LANDERS R, LAIB A, et al. Biofunctional rapid prototyping for tissue-engineering applications: 3D bioplotting versus 3D printing[J]. Journal of Polymer Science Part A: Polymer Chemistry, 2004, 42(3): 624-638. |
| 64 | LI S K, LI Z H, YANG J, et al. Inhibition of sympathetic activation by delivering calcium channel blockers from a 3D printed scaffold to promote bone defect repair[J]. Advanced Healthcare Materials, 2022, 11(16): e2200785. |
| 65 | MA X Y, QU X, ZHU W, et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(8): 2206-2211. |
| 66 | YAP K K, GERRAND Y W, DINGLE A M, et al. Liver sinusoidal endothelial cells promote the differentiation and survival of mouse vascularised hepatobiliary organoids[J]. Biomaterials, 2020, 251: 120091. |
| 67 | TSENG T C, HSIEH F Y, THEATO P, et al. Glucose-sensitive self-healing hydrogel as sacrificial materials to fabricate vascularized constructs[J]. Biomaterials, 2017, 133: 20-28. |
| 68 | HOSSEINI M, KOEHLER K R, SHAFIEE A. Biofabrication of human skin with its appendages[J]. Advanced Healthcare Materials, 2022, 11(22): e2201626. |
| 69 | VEDADGHAVAMI A, MINOOEI F, MOHAMMADI M H, et al. Manufacturing of hydrogel biomaterials with controlled mechanical properties for tissue engineering applications[J]. Acta Biomaterialia, 2017, 62: 42-63. |
| 70 | LIU H T, WANG Y Q, CUI K L, et al. Advances in hydrogels in organoids and organs-on-a-chip[J]. Advanced Materials, 2019, 31(50): e1902042. |
| 71 | KIM J, KIM J, GAO G, et al. Bioprinted organoids platform with tumor vasculature for implementing precision personalized medicine targeted towards gastric cancer[J]. Advanced Functional Materials, 2023: 2306676. |
| 72 | MORGAN J P, DELNERO P F, ZHENG Y, et al. Formation of microvascular networks in vitro [J]. Nature Protocols, 2013, 8(9): 1820-1836. |
| 73 | GRAÇA M F P, MIGUEL S P, CABRAL C S D, et al. Hyaluronic acid-Based wound dressings: a review[J]. Carbohydrate Polymers, 2020, 241: 116364. |
| 74 | WRAY L S, TSIORIS K, GI E S, et al. Slowly degradable porous silk microfabricated scaffolds for vascularized tissue formation[J]. Advanced Functional Materials, 2013, 23(27): 3404-3412. |
| 75 | LUO L L, LIU L B, DING Y X, et al. Advances in biomimetic hydrogels for organoid culture[J]. Chemical Communications, 2023, 59(64): 9675-9686. |
| 76 | ZHANG Y S, PI Q M, VAN GENDEREN A M. Microfluidic bioprinting for engineering vascularized tissues and organoids[J]. Journal of Visualized Experiments, 2017(126): e55957. |
| 77 | HUANG J J, XU Z Y, JIAO J, et al. Microfluidic intestinal organoid-on-a-chip uncovers therapeutic targets by recapitulating oxygen dynamics of intestinal IR injury[J]. Bioactive Materials, 2023, 30: 1-14. |
| 78 | DALY A C, CUNNIFFE G M, SATHY B N, et al. 3D bioprinting of developmentally inspired templates for whole bone organ engineering[J]. Advanced Healthcare Materials, 2016, 5(18): 2353-2362. |
| 79 | WANG H, LIU H T, LIU H, et al. One-step generation of core-shell gelatin methacrylate (GelMA) microgels using a droplet microfluidic system[J]. Advanced Materials Technologies, 2019, 4(6): 1800632. |
| 80 | GUO L Q, LIANG Z H, YANG L, et al. The role of natural polymers in bone tissue engineering[J]. Journal of Controlled Release, 2021, 338: 571-582. |
| 81 | ZHU B W, WANG D Z, PAN H P, et al. Three-in-one customized bioink for islet organoid: GelMA/ECM/PRP orchestrate pro-angiogenic and immunoregulatory function[J]. Colloids and Surfaces B, Biointerfaces, 2023, 221: 113017. |
| 82 | ESCUDERO M, VAYSSE L, EKE G, et al. Scalable generation of pre-vascularized and functional human beige adipose organoids[J]. Advanced Science, 2023, 10(31): e2301499. |
| 83 | SADR N, ZHU M J, OSAKI T, et al. SAM-based cell transfer to photopatterned hydrogels for microengineering vascular-like structures[J]. Biomaterials, 2011, 32(30): 7479-7490. |
| 84 | WANG D Z, GUO Y B, ZHU J C, et al. Hyaluronic acid methacrylate/pancreatic extracellular matrix as a potential 3D printing bioink for constructing islet organoids[J]. Acta Biomaterialia, 2023, 165: 86-101. |
| 85 | EKE G, MANGIR N, HASIRCI N, et al. Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering[J]. Biomaterials, 2017, 129: 188-198. |
| 86 | BARRY C, SCHMITZ M T, PROPSON N E, et al. Uniform neural tissue models produced on synthetic hydrogels using standard culture techniques[J]. Experimental Biology and Medicine, 2017, 242(17): 1679-1689. |
| 87 | MILLER J S, STEVENS K R, YANG M T, et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues[J]. Nature Materials, 2012, 11(9): 768-774. |
| 88 | WANG X X, WANG X S, LIU J J, et al. Hair follicle and sebaceous gland de novo regeneration with cultured epidermal stem cells and skin-derived precursors[J]. Stem Cells Translational Medicine, 2016, 5(12): 1695-1706. |
| 89 | CHACÓN-MARTÍNEZ C A, KLOSE M, NIEMANN C, et al. Hair follicle stem cell cultures reveal self-organizing plasticity of stem cells and theirprogeny[J]. The EMBO Journal, 2017, 36(2): 151-164. |
| 90 | ZHANG X Y, XIAO S E, LIU B C, et al. Use of extracellular matrix hydrogel from human placenta to restore hair-inductive potential of dermal papilla cells[J]. Regenerative Medicine, 2019, 14(8): 741-751. |
| 91 | YAO B, WANG R, WANG Y H, et al. Biochemical and structural cues of 3D-printed matrix synergistically direct MSC differentiation for functional sweat gland regeneration[J]. Science Advances, 2020, 6(10): eaaz1094. |
| 92 | NANMO A, YAN L, ASABA T, et al. Bioprinting of hair follicle germs for hair regenerative medicine[J]. Acta Biomaterialia, 2023, 165: 50-59. |
| 93 | BROGUIERE N, ISENMANN L, HIRT C, et al. Growth of epithelial organoids in a defined hydrogel[J]. Advanced Materials, 2018, 30(43): e1801621. |
| 94 | SOZZI E, KAJTEZ J, BRUZELIUS A, et al. Silk scaffolding drives self-assembly of functional and mature human brain organoids[J]. Frontiers in Cell and Developmental Biology, 2022, 10: 1023279. |
| 95 | KALABUSHEVA E, TERSKIKH V, VOROTELYAK E. Hair germ model in vitro via human postnatal keratinocyte-dermal papilla interactions: impact of hyaluronic acid[J]. Stem Cells International, 2017, 2017: 9271869. |
| 96 | KAGEYAMA T, YOSHIMURA C, MYASNIKOVA D, et al. Spontaneous hair follicle germ (HFG) formation in vitro, enabling the large-scale production of HFGs for regenerative medicine[J]. Biomaterials, 2018, 154: 291-300. |
| 97 | WANG R, WANG Y H, YAO B, et al. Redirecting differentiation of mammary progenitor cells by 3D bioprinted sweat gland microenvironment[J]. Burns & Trauma, 2019, 7: 29. |
| 98 | KRÜGER M, OOSTERHOFF L A, VAN WOLFEREN M E, et al. Cellulose nanofibril hydrogel promotes hepatic differentiation of human liver organoids[J]. Advanced Healthcare Materials, 2020, 9(6): e1901658. |
| 99 | NIE J, GAO Q, WANG Y D, et al. Vessel-on-a-chip with hydrogel-based microfluidics[J]. Small, 2018, 14(45): e1802368. |
| 100 | TENG Y Y, ZOU M L, LIU S Y, et al. Dual-action icariin-containing thermosensitive hydrogel for wound macrophage polarization and hair-follicle Neogenesis [J]. Frontiers in Bioengineering and Biotechnology, 2022, 10: 902894. |
| 101 | LI H H, CHEN L, ZENG S P, et al. Matrigel basement membrane matrix induces eccrine sweat gland cells to reconstitute sweat gland-like structures in nude mice[J]. Experimental Cell Research, 2015, 332(1): 67-77. |
| 102 | KAGEYAMA T, SHIMIZU A, ANAKAMA R, et al. Reprogramming of three-dimensional microenvironments for in vitro hair follicle induction[J]. Science Advances, 2022, 8(42): eadd4603. |
| 103 | SHI W, MIRZA S, KUSS M, et al. Embedded bioprinting of breast tumor cells and organoids using low-concentration collagen-based bioinks[J]. Advanced Healthcare Materials, 2023, 12(26): e2300905. |
| 104 | YAMANLAR S, SANT S, BOUDOU T, et al. Surface functionalization of hyaluronic acid hydrogels by polyelectrolyte multilayer films[J]. Biomaterials, 2011, 32(24): 5590-5599. |
| 105 | JEON E Y, SORRELLS L, ABACI H E. Biomaterials and bioengineering to guide tissue morphogenesis in epithelial organoids[J]. Frontiers in Bioengineering and Biotechnology, 2022, 10: 1038277. |
| 106 | LUTOLF M P, HUBBELL J A. Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering[J]. Nature Biotechnology, 2005, 23(1): 47-55. |
| 107 | TIBBITT M W, ANSETH K S. Hydrogels as extracellular matrix mimics for 3D cell culture[J]. Biotechnology and Bioengineering, 2009, 103(4): 655-663. |
| 108 | BADYLAK S F. The extracellular matrix as a scaffold for tissue reconstruction[J]. Seminars in Cell & Developmental Biology, 2002, 13(5): 377-383. |
| 109 | LI Y H, HAN Y, WANG X Y, et al. Multifunctional hydrogels prepared by dual ion cross-linking for chronic wound healing[J]. ACS Applied Materials & Interfaces, 2017, 9(19): 16054-16062. |
| 110 | NGUYEN E H, DALY W T, LE N N T, et al. Versatile synthetic alternatives to Matrigel for vascular toxicity screening and stem cell expansion[J]. Nature Biomedical Engineering, 2017, 1: 0096. |
| 111 | HOSSEINI M, SHAFIEE A. Engineering bioactive scaffolds for skin regeneration[J]. Small, 2021, 17(41): e2101384. |
| 112 | CARMELIET P, JAIN R K. Molecular mechanisms and clinical applications of angiogenesis[J]. Nature, 2011, 473(7347): 298-307. |
| 113 | NOLAN D J, GINSBERG M, ISRAELY E, et al. Molecular signatures of tissue-specific microvascular endothelial cell heterogeneity in organ maintenance and regeneration[J]. Developmental Cell, 2013, 26(2): 204-219. |
| 114 | LI X R, CARMELIET P. Targeting angiogenic metabolism in disease[J]. Science, 2018, 359(6382): 1335-1336. |
| 115 | TEUWEN L A, DRAOUI N, DUBOIS C, et al. Endothelial cell metabolism: an update anno 2017[J]. Current Opinion in Hematology, 2017, 24(3): 240-247. |
| 116 | AUGUSTIN H G, KOH G Y. Organotypic vasculature: from descriptive heterogeneity to functional pathophysiology[J]. Science, 2017, 357(6353): eaal2379. |
| 117 | REITERER M, BRANCO C M. Endothelial cells and organ function: applications and implications of understanding unique and reciprocal remodelling[J]. The FEBS Journal, 2020, 287(6): 1088-1100. |
| 118 | TRIMM E, RED-HORSE K. Vascular endothelial cell development and diversity[J]. Nature Reviews Cardiology, 2023, 20(3): 197-210. |
| 119 | CHOW B W, GU C H. The molecular constituents of the blood-brain barrier[J]. Trends in Neurosciences, 2015, 38(10): 598-608. |
| 120 | ITKIN T, GUR-COHEN S, SPENCER J A, et al. Distinct bone marrow blood vessels differentially regulate haematopoiesis[J]. Nature, 2016, 532(7599): 323-328. |
| 121 | RAJABI M, MOUSA S A. The role of angiogenesis in cancer treatment[J]. Biomedicines, 2017, 5(2): 34. |
| 122 | ILIFF A J, XU X Z S. A mechanosensitive GPCR that detects the bloody force[J]. Cell, 2018, 173(3): 542-544. |
| 123 | DE BOCK K, GEORGIADOU M, SCHOORS S, et al. Role of PFKFB3-driven glycolysis in vessel sprouting[J]. Cell, 2013, 154(3): 651-663. |
| 124 | POTENTE M, CARMELIET P. The link between angiogenesis and endothelial metabolism[J]. Annual Review of Physiology, 2017, 79: 43-66. |
| 125 | YUAN L, XIE S F, BAI H R, et al. Reconstruction of dynamic mammary mini gland in vitro for normal physiology and oncogenesis[J]. Nature Methods, 2023, 20(12): 2021-2033. |
| 126 | CHEN Y W, HUANG S X, DE CARVALHO A L R T, et al. A three-dimensional model of human lung development and disease from pluripotent stem cells[J]. Nature Cell Biology, 2017, 19(5): 542-549. |
| 127 | CAPOWSKI E E, SAMIMI K, MAYERL S J, et al. Reproducibility and staging of 3D human retinal organoids across multiple pluripotent stem cell lines[J]. Development, 2019, 146(1): dev171686. |
| 128 | PHIPSON B, ER P X, COMBES A N, et al. Evaluation of variability in human kidney organoids[J]. Nature Methods, 2019, 16(1): 79-87. |
| [1] | HONG Yuan, LIU Yan. Research progress of brain organoids in regenerative medicine [J]. Synthetic Biology Journal, 2024, 5(4): 754-769. |
| [2] | Qianwen CHEN, Siqi ZHAO, Yaojin PENG. Organoids: technological innovation and ethical controversies [J]. Synthetic Biology Journal, 2024, 5(4): 898-907. |
| [3] | ZHANG Bohang, QI Xiaoxuan, YUAN Yan. Advancements in testicular organoids for in vitro spermatogenesis [J]. Synthetic Biology Journal, 2024, 5(4): 770-781. |
| [4] | HAN Yizhao, GUO Jia, SHAO Yue. Stem cell-based synthetic development: cellular components, embryonic models, and engineering approaches [J]. Synthetic Biology Journal, 2024, 5(4): 734-753. |
| [5] | Ke’er HU, Hanqi WANG, Ruqi HUANG, Canyang ZHANG, Xinhui XING, Shaohua MA. Integrated design strategies for engineered organoids and organ-on-a-chip technologies [J]. Synthetic Biology Journal, 2024, 5(4): 883-897. |
| [6] | AI Zongyong, ZHANG Chengting, NIU Baohua, YIN Yu, YANG Jie, LI Tianqing. Early human embryo development and stem cells [J]. Synthetic Biology Journal, 2024, 5(4): 700-718. |
| [7] | Liyu ZHU, Yulong ZHAO, Wei LI, Libin WANG. Progress in mammalian chromosome engineering [J]. Synthetic Biology Journal, 2023, 4(2): 394-406. |
| [8] | Jingjing LI, Chao MA, Fan WANG, Hongjie ZHANG, Kai LIU. Biosynthesis of high-performance protein materials and their applications [J]. Synthetic Biology Journal, 2022, 3(4): 638-657. |
| [9] | Can ZHANG, Liyang SHI, Jianwu DAI. Cultured meat from biomaterials: challenges and prospects [J]. Synthetic Biology Journal, 2022, 3(4): 676-689. |
| [10] | Zhaoying YANG, Fan ZHANG, Jianwen GUO, Weiping GAO. Biosynthesis of elastin-like polypeptides and their applications in drug delivery [J]. Synthetic Biology Journal, 2022, 3(4): 728-747. |
| [11] | Botao JI, Zhigang QIAN, Xiaoxia XIA. Application of cell-free synthesis strategy in biomaterial research [J]. Synthetic Biology Journal, 2022, 3(4): 658-675. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||