Synthetic Biology Journal ›› 2024, Vol. 5 ›› Issue (4): 831-850.DOI: 10.12211/2096-8280.2024-044
• Invited Review • Previous Articles Next Articles
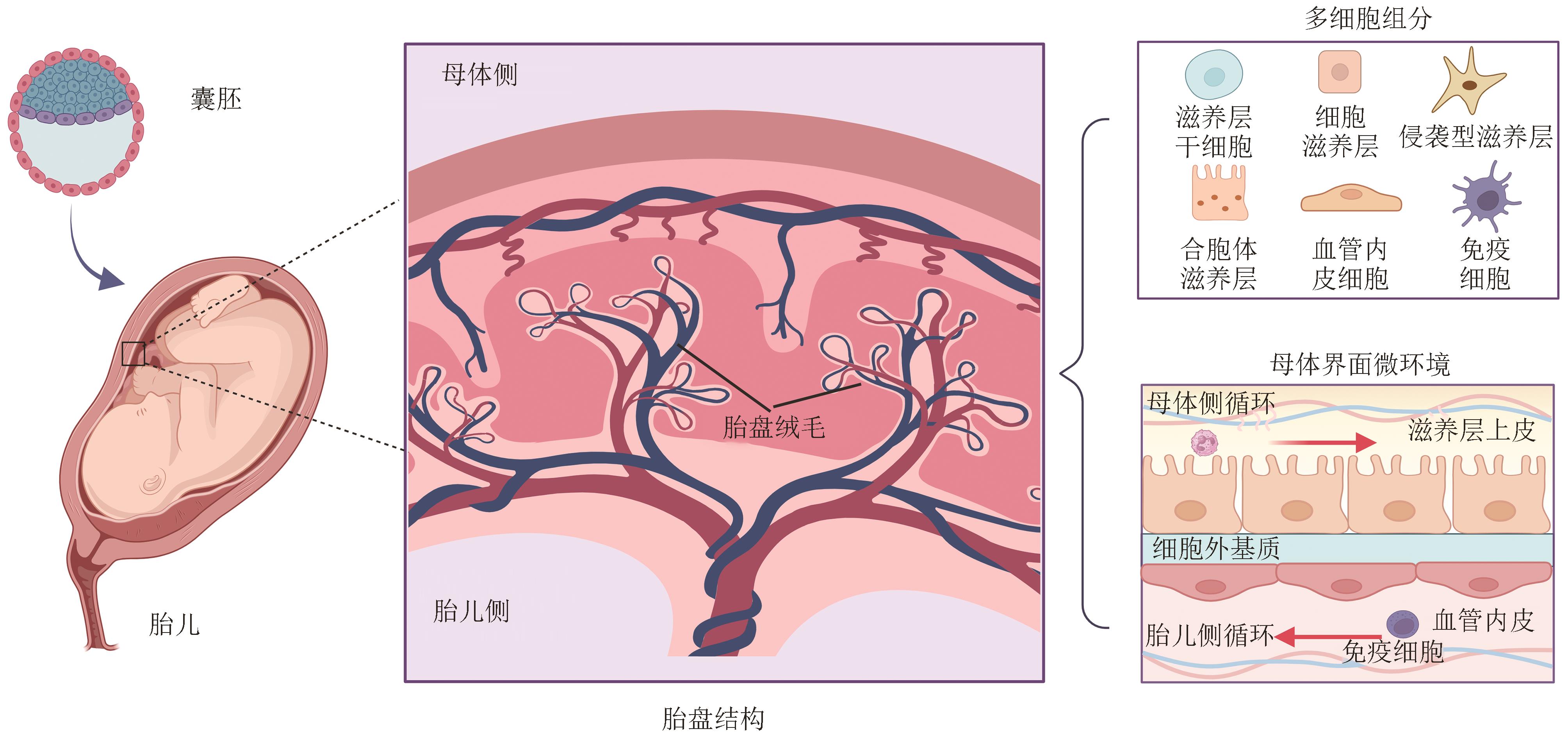
Advances in placenta-on-a-chip for reproductive medicine research
CAO Rongkai1,2, QIN Jianhua1, WANG Yaqing3,4
- 1.Dalian Institute of Chemical Physics,Chinese Academy of Sciences,Dalian 116023,Liaoning,China
2.University of Chinese Academy of Sciences,Beijing 100049,China
3.University of Science and Technology of China,Hefei 230026,Anhui,China
4.Suzhou Institute for Advanced Research,University of Science and Technology of China,Suzhou 215123,Jiangsu,China
-
Received:2024-05-30Revised:2024-06-25Online:2024-09-19Published:2024-08-31 -
Contact:WANG Yaqing
胎盘芯片及其在生殖医学领域的研究进展
曹荣凯1,2, 秦建华1, 王亚清3,4
- 1.中国科学院大连化学物理研究所,辽宁 大连 116023
2.中国科学院大学,北京 100049
3.中国科学技术大学,安徽 合肥 230026
4.中国科学技术大学苏州高等研究院,江苏 苏州 215123
-
通讯作者:王亚清 -
作者简介:曹荣凯 (1996—),男,博士研究生。研究方向为人胎盘模型的体外构建及其在生物医学领域的应用。E-mail:caorongkai@dicp.ac.cn王亚清 (1989—),女,博士,副研究员。研究方向为类器官工程及其生物医学应用。E-mail:wangyaqing@ustc.edu.cn -
基金资助:国家自然科学基金(32301206);国家重点研发计划(2022YFA1104700)
CLC Number:
Cite this article
CAO Rongkai, QIN Jianhua, WANG Yaqing. Advances in placenta-on-a-chip for reproductive medicine research[J]. Synthetic Biology Journal, 2024, 5(4): 831-850.
曹荣凯, 秦建华, 王亚清. 胎盘芯片及其在生殖医学领域的研究进展[J]. 合成生物学, 2024, 5(4): 831-850.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://synbioj.cip.com.cn/EN/10.12211/2096-8280.2024-044
| 1 | KNÖFLER M, HAIDER S, SALEH L, et al. Human placenta and trophoblast development: key molecular mechanisms and model systems[J]. Cellular and Molecular Life Sciences, 2019, 76(18): 3479-3496. |
| 2 | ROSENFELD C S. Transcriptomics and other omics approaches to investigate effects of xenobiotics on the placenta[J]. Frontiers in Cell and Developmental Biology, 2021, 9: 723656. |
| 3 | ANDER S E, DIAMOND M S, COYNE C B. Immune responses at the maternal-fetal interface[J]. Science Immunology, 2019, 4(31): eaat6114. |
| 4 | BROSENS I, PIJNENBORG R, VERCRUYSSE L, et al. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation[J]. American Journal of Obstetrics and Gynecology, 2011, 204(3): 193-201. |
| 5 | KRISHNA U, BHALERAO S. Placental insufficiency and fetal growth restriction[J]. Journal of Obstetrics and Gynaecology of India, 2011, 61(5): 505-511. |
| 6 | SMITH G C S. First-trimester determination of complications of late pregnancy[J]. The Journal of the American Medical Association, 2010, 303(6): 561-562. |
| 7 | SCHMIDT A, MORALES-PRIETO D M, PASTUSCHEK J, et al. Only humans have human placentas: molecular differences between mice and humans[J]. Journal of Reproductive Immunology, 2015, 108: 65-71. |
| 8 | CHAOUAT G, CLARK D A. Are animal models useful or confusing in understanding the human feto-maternal relationship? A debate[J]. Journal of Reproductive Immunology, 2015, 108: 56-64. |
| 9 | AUBUCHON M, SCHULZ L C, SCHUST D J. Preeclampsia: animal models for a human cure[J]. Proceedings of the National Academy of Sciences of the United States of America, 2011, 108(4): 1197-1198. |
| 10 | MCCARTHY F P, KINGDOM J C, KENNY L C, et al. Animal models of preeclampsia; uses and limitations[J]. Placenta, 2011, 32(6): 413-419. |
| 11 | ROTHBAUER M, PATEL N, GONDOLA H, et al. A comparative study of five physiological key parameters between four different human trophoblast-derived cell lines[J]. Scientific Reports, 2017, 7(1): 5892. |
| 12 | ABBAS Y, TURCO M Y, BURTON G J, et al. Investigation of human trophoblast invasion in vitro [J]. Human Reproduction Update, 2020, 26(4): 501-513. |
| 13 | CONINGS S, AMANT F, ANNAERT P, et al. Integration and validation of the ex vivo human placenta perfusion model[J]. Journal of Pharmacological and Toxicological Methods, 2017, 88(Pt 1): 25-31. |
| 14 | MYLLYNEN P, MATHIESEN L, WEIMER M, et al. Preliminary interlaboratory comparison of the ex vivo dual human placental perfusion system[J]. Reproductive Toxicology, 2010, 30(1): 94-102. |
| 15 | ORENDI K, KIVITY V, SAMMAR M, et al. Placental and trophoblastic in vitro models to study preventive and therapeutic agents for preeclampsia[J]. Placenta, 2011, 32(): S49-S54. |
| 16 | XIAO Z Y, YAN L, LIANG X Y, et al. Progress in deciphering trophoblast cell differentiation during human placentation[J]. Current Opinion in Cell Biology, 2020, 67: 86-91. |
| 17 | WONG F, COX B J. Cellular analysis of trophoblast and placenta[J]. Placenta, 2017, 59: S2-S7. |
| 18 | LI L P, SCHUST D J. Isolation, purification and in vitro differentiation of cytotrophoblast cells from human term placenta[J]. Reproductive Biology and Endocrinology, 2015, 13: 71. |
| 19 | VARDHANA P A, ILLSLEY N P. Transepithelial glucose transport and metabolism in BeWo choriocarcinoma cells[J]. Placenta, 2002, 23(8-9): 653-660. |
| 20 | FUCHS R, ELLINGER I. Endocytic and transcytotic processes in villous syncytiotrophoblast: role in nutrient transport to the human fetus[J]. Traffic, 2004, 5(10): 725-738. |
| 21 | MARTINEZ F, OLVERA-SANCHEZ S, ESPARZA-PERUSQUIA M, et al. Multiple functions of syncytiotrophoblast mitochondria[J]. Steroids, 2015, 103: 11-22. |
| 22 | COSTA M A. The endocrine function of human placenta: an overview[J]. Reproductive BioMedicine Online, 2016, 32(1): 14-43. |
| 23 | PIJNENBORG R, DIXON G, ROBERTSON W B, et al. Trophoblastic invasion of human decidua from 8 to 18 weeks of pregnancy[J]. Placenta, 1980, 1(1): 3-19. |
| 24 | HE N N, VAN IPEREN L, JONG D D, et al. Human extravillous trophoblasts penetrate decidual veins and lymphatics before remodeling spiral arteries during early pregnancy[J]. PLoS One, 2017, 12(1): e0169849. |
| 25 | MORLEY L C, BEECH D J, WALKER J J, et al. Emerging concepts of shear stress in placental development and function[J]. Molecular Human Reproduction, 2019, 25(6): 329-339. |
| 26 | CHANG C W, WAKELAND A K, PARAST M M. Trophoblast lineage specification, differentiation and their regulation by oxygen tension[J]. The Journal of Endocrinology, 2018, 236(1): R43-R56. |
| 27 | ROBERTS V H J, MORGAN T K, BEDNAREK P, et al. Early first trimester uteroplacental flow and the progressive disintegration of spiral artery plugs: new insights from contrast-enhanced ultrasound and tissue histopathology[J]. Human Reproduction, 2017, 32(12): 2382-2393. |
| 28 | WEISS G, SUNDL M, GLASNER A, et al. The trophoblast plug during early pregnancy: a deeper insight[J]. Histochemistry and Cell Biology, 2016, 146(6): 749-756. |
| 29 | JAMES J L, WHITLEY G S, CARTWRIGHT J E. Shear stress and spiral artery remodelling: the effects of low shear stress on trophoblast-induced endothelial cell apoptosis[J]. Cardiovascular Research, 2011, 90(1): 130-139. |
| 30 | BURTON G J, CINDROVA-DAVIES T, YUNG H W, et al. Hypoxia and reproductive health: oxygen and development of the human placenta[J]. Reproduction, 2021, 161(1): F53-F65. |
| 31 | JAMES J L, SAGHIAN R, PERWICK R, et al. Trophoblast plugs: impact on utero-placental haemodynamics and spiral artery remodelling[J]. Human Reproduction, 2018, 33(8): 1430-1441. |
| 32 | JAUNIAUX E, WATSON A L, HEMPSTOCK J, et al. Onset of maternal arterial blood flow and placental oxidative stress. A possible factor in human early pregnancy failure[J]. The American Journal of Pathology, 2000, 157(6): 2111-2122. |
| 33 | BURTON G J, WOODS A W, JAUNIAUX E, et al. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy[J]. Placenta, 2009, 30(6): 473-482. |
| 34 | BURTON G J, REDMAN C W, ROBERTS J M, et al. Pre-eclampsia: pathophysiology and clinical implications[J]. British Medical Journal, 2019, 366: l2381. |
| 35 | ROTH C J, HAEUSSNER E, RUEBELMANN T, et al. Dynamic modeling of uteroplacental blood flow in IUGR indicates vortices and elevated pressure in the intervillous space - a pilot study[J]. Scientific Reports, 2017, 7: 40771. |
| 36 | AL-NASIRY S, SPITZ B, HANSSENS M, et al. Differential effects of inducers of syncytialization and apoptosis on BeWo and JEG-3 choriocarcinoma cells[J]. Human Reproduction, 2006, 21(1): 193-201. |
| 37 | KNYAZEV E N, NIKULIN S V, KHRISTICHENKO A Y, et al. Transport and toxicity of 5-fluorouracil, doxorubicin, and cyclophosphamide in in vitro placental barrier model based on BeWo b30 cells[J]. Russian Chemical Bulletin, 2019, 68(12): 2344-2349. |
| 38 | KLOET S K, WALCZAK A P, LOUISSE J, et al. Translocation of positively and negatively charged polystyrene nanoparticles in an in vitro placental model[J]. Toxicology in Vitro, 2015, 29(7): 1701-1710. |
| 39 | KAWAMURA E, HAMILTON G B, MISKIEWICZ E I, et al. Examination of FERMT1 expression in placental chorionic villi and its role in HTR8-SVneo cell invasion[J]. Histochemistry and Cell Biology, 2021, 155(6): 669-681. |
| 40 | NONG Y Q, LI S F, LIU W J, et al. Aquaporin 3 promotes human extravillous trophoblast migration and invasion[J]. Reproductive Biology and Endocrinology, 2021, 19(1): 49. |
| 41 | NURSALIM Y N S, GROOM K M, BLENKIRON C, et al. A simple method to isolate term trophoblasts and maintain them in extended culture[J]. Placenta, 2021, 108: 1-10. |
| 42 | CASTEL G, MEISTERMANN D, BRETIN B, et al. Induction of human trophoblast stem cells from somatic cells and pluripotent stem cells[J]. Cell Reports, 2020, 33(8): 108419. |
| 43 | LIU X D, OUYANG J F, ROSSELLO F J, et al. Reprogramming roadmap reveals route to human induced trophoblast stem cells[J]. Nature, 2020, 586(7827): 101-107. |
| 44 | WEI Y X, WANG T Y, MA L S, et al. Efficient derivation of human trophoblast stem cells from primed pluripotent stem cells[J]. Science Advances, 2021, 7(33): eabf4416. |
| 45 | NAAMA M, RAHAMIM M, ZAYAT V, et al. Pluripotency-independent induction of human trophoblast stem cells from fibroblasts[J]. Nature Communications, 2023, 14(1): 3359. |
| 46 | OKAE H, TOH H, SATO T, et al. Derivation of human trophoblast stem cells[J]. Cell Stem Cell, 2018, 22(1): 50-63.e6. |
| 47 | LEE J S, ROMERO R, HAN Y M, et al. Placenta-on-a-chip: a novel platform to study the biology of the human placenta[J]. The Journal of Maternal-Fetal & Neonatal Medicine, 2016, 29(7): 1046-1054. |
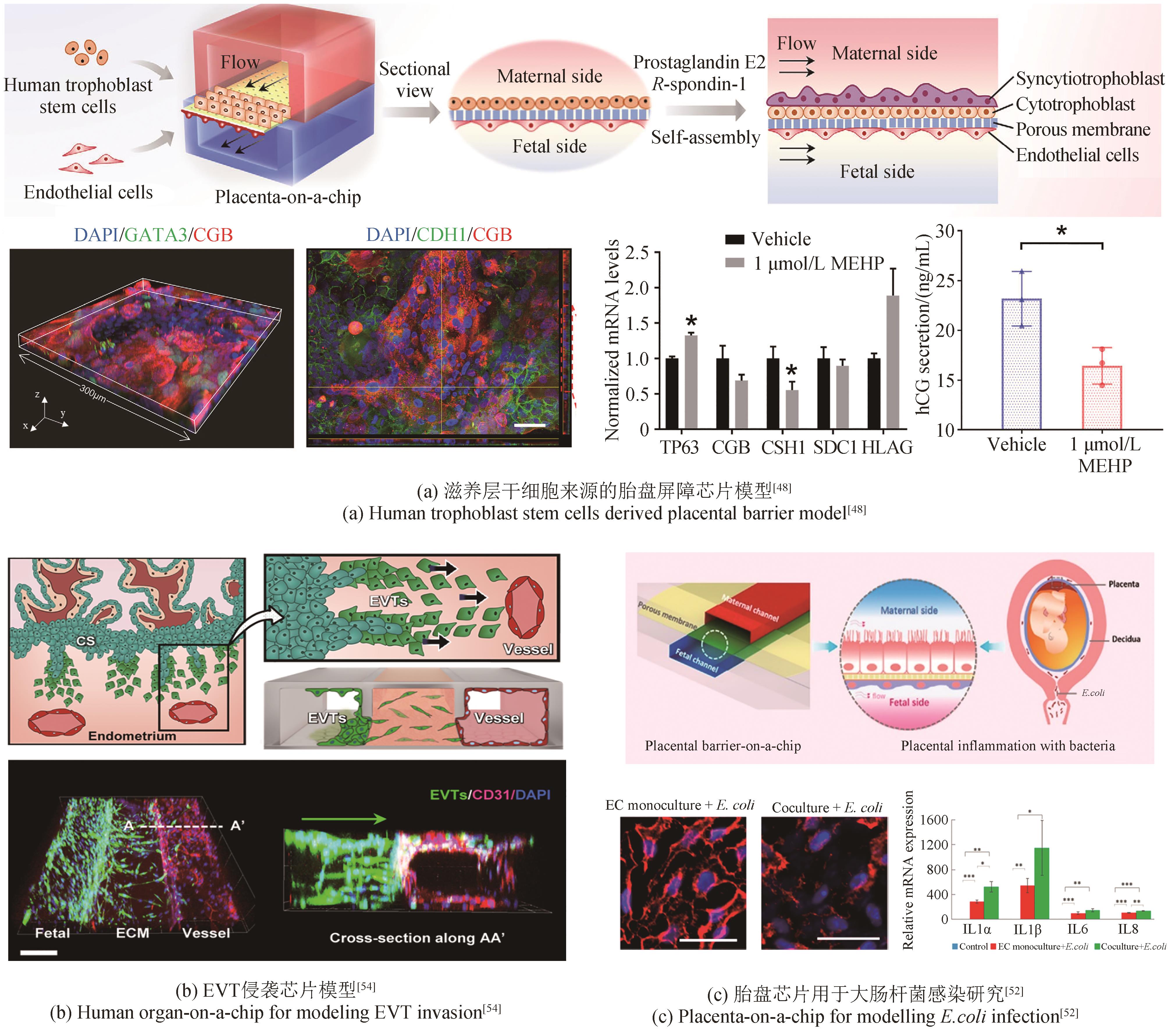
| 48 | CAO R K, WANG Y Q, LIU J Y, et al. Self-assembled human placental model from trophoblast stem cells in a dynamic organ-on-a-chip system[J]. Cell Proliferation, 2023, 56(5): e13469. |
| 49 | BLUNDELL C, YI Y S, MA L, et al. Placental drug transport-on-a-chip: a microengineered in vitro model of transporter-mediated drug efflux in the human placental barrier[J]. Advanced Healthcare Materials, 2018, 7(2): 1700786. |
| 50 | BLUNDELL C, TESS E R, SCHANZER A S, et al. A microphysiological model of the human placental barrier[J]. Lab on a Chip, 2016, 16(16): 3065-3073. |
| 51 | YIN F C, ZHU Y J, ZHANG M, et al. A 3D human placenta-on-a-chip model to probe nanoparticle exposure at the placental barrier[J]. Toxicology in Vitro, 2019, 54: 105-113. |
| 52 | ZHU Y J, YIN F C, WANG H, et al. Placental barrier-on-a-chip: modeling placental inflammatory responses to bacterial infection[J]. ACS Biomaterials Science & Engineering, 2018, 4(9): 3356-3363. |
| 53 | LI Q, SHARKEY A, SHERIDAN M, et al. Human uterine natural killer cells regulate differentiation of extravillous trophoblast early in pregnancy[J]. Cell Stem Cell, 2024, 31(2): 181-195.e9. |
| 54 | PARK J Y, MANI S, CLAIR G, et al. A microphysiological model of human trophoblast invasion during implantation[J]. Nature Communications, 2022, 13(1): 1252. |
| 55 | HIGHET A R, KHODA S M, BUCKBERRY S, et al. Hypoxia induced HIF-1/HIF-2 activity alters trophoblast transcriptional regulation and promotes invasion[J]. European Journal of Cell Biology, 2015, 94(12): 589-602. |
| 56 | WONG M K, LI E W, ADAM M, et al. Establishment of an in vitro placental barrier model cultured under physiologically relevant oxygen levels[J]. Molecular Human Reproduction, 2020, 26(5): 353-365. |
| 57 | HU X Q, ZHANG L B. Hypoxia and mitochondrial dysfunction in pregnancy complications[J]. Antioxidants, 2021, 10(3): 405. |
| 58 | WOO J H, LEE I, KIM S M, et al. Recapitulation of trophoblast invasion during pregnancy in a physiological hypoxia induced microfluidic device[C/OL]//ASME-JSME-KSME 2019 8th Joint Fluids Engineering Conference, July 28–August 1, 2019, San Francisco, California, USA.(2019-11-20)[2024-03-01]. . |
| 59 | LECARPENTIER E, BHATT M, BERTIN G I, et al. Computational fluid dynamic simulations of maternal circulation: wall shear stress in the human placenta and its biological implications[J]. PLoS One, 2016, 11(1): e0147262. |
| 60 | BRUGGER B A, GUETTLER J, GAUSTER M. Go with the flow-trophoblasts in flow culture[J]. International Journal of Molecular Sciences, 2020, 21(13): 4666. |
| 61 | MIURA S, SATO K, KATO-NEGISHI M, et al. Fluid shear triggers microvilli formation via mechanosensitive activation of TRPV6[J]. Nature Communications, 2015, 6: 8871. |
| 62 | SANZ G, DANIEL N, AUBRIÈRE M C, et al. Differentiation of derived rabbit trophoblast stem cells under fluid shear stress to mimic the trophoblastic barrier[J]. Biochimica et Biophysica Acta General Subjects, 2019, 1863(10): 1608-1618. |
| 63 | HOLDER B S, TOWER C L, JONES C J, et al. Heightened pro-inflammatory effect of preeclamptic placental microvesicles on peripheral blood immune cells in humans[J]. Biology of Reproduction, 2012, 86(4): 103. |
| 64 | JONES C J P, FOX H. An ultrastructural and ultrahistochemical study of the human placenta in maternal pre-eclampsia[J]. Placenta, 1980, 1(1): 61-76. |
| 65 | RIQUELME G, VALLEJOS C, GREGORIO N D, et al. Lipid rafts and cytoskeletal proteins in placental microvilli membranes from preeclamptic and IUGR pregnancies[J]. The Journal of Membrane Biology, 2011, 241(3): 127-140. |
| 66 | ARISHE O O, EBEIGBE A B, WEBB R C. Mechanotransduction and uterine blood flow in preeclampsia: the role of mechanosensing Piezo 1 ion channels[J]. American Journal of Hypertension, 2020, 33(1): 1-9. |
| 67 | MA Z W, SAGRILLO-FAGUNDES L, MOK S, et al. Mechanobiological regulation of placental trophoblast fusion and function through extracellular matrix rigidity[J]. Scientific Reports, 2020, 10(1): 5837. |
| 68 | NABA A. TenYears of extracellular matrix proteomics: accomplishments, challenges, and future perspectives[J]. Molecular & Cellular Proteomics, 2023, 22(4): 100528. |
| 69 | NISHIGUCHI A, GILMORE C, SOOD A, et al. In vitro placenta barrier model using primary human trophoblasts, underlying connective tissue and vascular endothelium[J]. Biomaterials, 2019, 192: 140-148. |
| 70 | ZAMBUTO S G, RATTILA S, DVEKSLER G, et al. Effects of pregnancy-specific glycoproteins on trophoblast motility in three-dimensional gelatin hydrogels[J]. Cellular and Molecular Bioengineering, 2022, 15(2): 175-191. |
| 71 | MANDT D, GRUBER P, MARKOVIC M, et al. Fabrication of biomimetic placental barrier structures within a microfluidic device utilizing two-photon polymerization[J]. International Journal of Bioprinting, 2018, 4(2): 144. |
| 72 | WONG M K, SHAWKY S A, ARYASOMAYAJULA A, et al. Extracellular matrix surface regulates self-assembly of three-dimensional placental trophoblast spheroids[J]. PLoS One, 2018, 13(6): e0199632. |
| 73 | ABBAS Y, CARNICER-LOMBARTE A, GARDNER L, et al. Tissue stiffness at the human maternal-fetal interface[J]. Human Reproduction, 2019, 34(10): 1999-2008. |
| 74 | SHOJAEI S, ALI M S, SURESH M, et al. Dynamic placenta-on-a-chip model for fetal risk assessment of nanoparticles intended to treat pregnancy-associated diseases[J]. Biochimica et Biophysica Acta Molecular Basis of Disease, 2021, 1867(7): 166131. |
| 75 | ARUMUGASAAMY N, ROCK K D, KUO C Y, et al. Microphysiological systems of the placental barrier[J]. Advanced Drug Delivery Reviews, 2020, 161-162: 161-175. |
| 76 | KAZEMIAN A, HOOSHMANDABBASI R, SCHRANER E M, et al. Evolutionary implications of fetal and maternal microvillous surfaces in epitheliochorial placentae[J]. Journal of Morphology, 2019, 280(4): 615-622. |
| 77 | TUTAR R, ÇELEBI-SALTIK B. Modeling of artificial 3D human placenta[J]. Cells, Tissues, Organs, 2022, 211(4): 527-536. |
| 78 | LEACH L. The phenotype of the human materno-fetal endothelial barrier: molecular occupancy of paracellular junctions dictate permeability and angiogenic plasticity[J]. Journal of Anatomy, 2002, 200(6): 599-606. |
| 79 | MOORE K H, MURPHY H A, CHAPMAN H, et al. Syncytialization alters the extracellular matrix and barrier function of placental trophoblasts[J]. American Journal of Physiology Cell Physiology, 2021, 321(4): C694-C703. |
| 80 | WALKER N, FILIS P, SOFFIENTINI U, et al. Placental transporter localization and expression in the Human: the importance of species, sex, and gestational age differences[J]. Biology of Reproduction, 2017, 96(4): 733-742. |
| 81 | EVAIN-BRION D, MALASSINE A. Human placenta as an endocrine organ[J]. Growth Hormone & IGF Research, 2003, 13: S34-S37. |
| 82 | D’HAUTERIVE S P, CLOSE R, GRIDELET V, et al. Human chorionic gonadotropin and early embryogenesis: review[J]. International Journal of Molecular Sciences, 2022, 23(3): 1380. |
| 83 | ZHANG N, WANG W S, LI W J, et al. Reduction of progesterone, estradiol and hCG secretion by perfluorooctane sulfonate via induction of apoptosis in human placental syncytiotrophoblasts[J]. Placenta, 2015, 36(5): 575-580. |
| 84 | ROGERS L M, HUGGINS M, DOSTER R S, et al. Impact of metabolic stress on BeWo syncytiotrophoblast function[J]. ChemBioChem, 2023, 24(24): e202300410. |
| 85 | BHATIA S N, INGBER D E. Microfluidic organs-on-chips[J]. Nature Biotechnology, 2014, 32: 760-772. |
| 86 | RENNERT K, STEINBORN S, GRÖGER M, et al. A microfluidically perfused three dimensional human liver model[J]. Biomaterials, 2015, 71: 119-131. |
| 87 | KIM H J, LI H, COLLINS J J, et al. Contributions of microbiome and mechanical deformation to intestinal bacterial overgrowth and inflammation in a human gut-on-a-chip[J]. Proceedings of the National Academy of Sciences of the United States of America, 2016, 113(1): E7-E15. |
| 88 | MAOZ B M, HERLAND A, FITZGERALD E A, et al. A linked organ-on-chip model of the human neurovascular unit reveals the metabolic coupling of endothelial and neuronal cells[J]. Nature Biotechnology, 2018, 36(9): 865-874. |
| 89 | HUH D, MATTHEWS B D, MAMMOTO A, et al. Reconstituting organ-level lung functions on a chip[J]. Science, 2010, 328(5986): 1662-1668. |
| 90 | PU Y, GINGRICH J, VEIGA-LOPEZ A. A 3-dimensional microfluidic platform for modeling human extravillous trophoblast invasion and toxicological screening[J]. Lab on a Chip, 2021, 21(3): 546-557. |
| 91 | ABBAS Y, OEFNER C M, POLACHECK W J, et al. A microfluidics assay to study invasion of human placental trophoblast cells[J]. Journal of the Royal Society, Interface, 2017, 14(130): 20170131. |
| 92 | ZHANG W J, LI J W, ZHOU J Q, et al. Translational organoid technology - the convergence of chemical, mechanical, and computational biology[J]. Trends in Biotechnology, 2022, 40(9): 1121-1135. |
| 93 | TURCO M Y, GARDNER L, KAY R G, et al. Trophoblast organoids as a model for maternal-fetal interactions during human placentation[J]. Nature, 2018, 564(7735): 263-267. |
| 94 | HAIDER S, MEINHARDT G, SALEH L, et al. Self-renewing trophoblast organoids recapitulate the developmental program of the early human placenta[J]. Stem Cell Reports, 2018, 11(2): 537-551. |
| 95 | SHERIDAN M A, FERNANDO R C, GARDNER L, et al. Establishment and differentiation of long-term trophoblast organoid cultures from the human placenta[J]. Nature Protocols, 2020, 15(10): 3441-3463. |
| 96 | YANG L H, LIANG P F, YANG H H, et al. Trophoblast organoids with physiological polarity model placental structure and function[J]. Journal of Cell Science, 2024, 137(5): jcs261528. |
| 97 | HORI T, OKAE H, SHIBATA S, et al. Trophoblast stem cell-based organoid models of the human placental barrier[J]. Nature Communications, 2024, 15(1): 962. |
| 98 | IO S, KABATA M, IEMURA Y, et al. Capturing human trophoblast development with naive pluripotent stem cells in vitro [J]. Cell Stem Cell, 2021, 28(6): 1023-1039.e13. |
| 99 | SONCIN F, MOREY R, BUI T, et al. Derivation of functional trophoblast stem cells from primed human pluripotent stem cells[J]. Stem Cell Reports, 2022, 17(6): 1303-1317. |
| 100 | HUANG L J, TU Z W, WEI L D, et al. Generating functional multicellular organoids from human placenta villi[J]. Advanced Science, 2023, 10(26): e2301565. |
| 101 | CUI K L, ZHU Y J, SHI Y, et al. Establishment of trophoblast-like tissue model from human pluripotent stem cells in three-dimensional culture system[J]. Advanced Science, 2022, 9(3): e2100031. |
| 102 | DENG P W, CUI K L, SHI Y, et al. Fluidic flow enhances the differentiation of placental trophoblast-like 3D tissue from hiPSCs in a perfused macrofluidic device[J]. Frontiers in Bioengineering and Biotechnology, 2022, 10: 907104. |
| 103 | TURCO M Y, GARDNER L, HUGHES J, et al. Long-term, hormone-responsive organoid cultures of human endometrium in a chemically defined medium[J]. Nature Cell Biology, 2017, 19(5): 568-577. |
| 104 | MCCONKEY C A, DELORME-AXFORD E, NICKERSON C A, et al. A three-dimensional culture system recapitulates placental syncytiotrophoblast development and microbial resistance[J]. Science Advances, 2016, 2(3): e1501462. |
| 105 | LEVKOVITZ R, ZARETSKY U, GORDON Z, et al. In vitro simulation of placental transport: part Ⅰ. Biological model of the placental barrier[J]. Placenta, 2013, 34(8): 699-707. |
| 106 | LEVKOVITZ R, ZARETSKY U, JAFFA A J, et al. In vitro simulation of placental transport: part Ⅱ. Glucose transfer across the placental barrier model[J]. Placenta, 2013, 34(8): 708-715. |
| 107 | KUO C Y, ERANKI A, PLACONE J K, et al. Development of a 3D printed, bioengineered placenta model to evaluate the role of trophoblast migration in preeclampsia[J]. ACS Biomaterials Science & Engineering, 2016, 2(10): 1817-1826. |
| 108 | KUO C Y, GUO T, CABRERA-LUQUE J, et al. Placental basement membrane proteins are required for effective cytotrophoblast invasion in a three-dimensional bioprinted placenta model[J]. Journal of Biomedical Materials Research Part A, 2018, 106(6): 1476-1487. |
| 109 | KUO C Y, SHEVCHUK M, OPFERMANN J, et al. Trophoblast-endothelium signaling involves angiogenesis and apoptosis in a dynamic bioprinted placenta model[J]. Biotechnology and Bioengineering, 2019, 116(1): 181-192. |
| 110 | GOLDSTEIN J A, GALLAGHER K, BECK C, et al. Maternal-fetal inflammation in the placenta and the developmental origins of health and disease[J]. Frontiers in Immunology, 2020, 11: 531543. |
| 111 | HUPPERTZ B. The critical role of abnormal trophoblast development in the etiology of preeclampsia[J]. Current Pharmaceutical Biotechnology, 2018, 19(10): 771-780. |
| 112 | NIRUPAMA R, DIVYASHREE S, JANHAVI P, et al. Preeclampsia: pathophysiology and management[J]. Journal of Gynecology Obstetrics and Human Reproduction, 2021, 50(2): 101975. |
| 113 | MELCHIORRE K, GIORGIONE V, THILAGANATHAN B. The placenta and preeclampsia: villain or victim?[J]. American Journal of Obstetrics and Gynecology, 2022, 226(2S): S954-S962. |
| 114 | GHORBANPOUR S M, RICHARDS C, PIENAAR D, et al. A placenta-on-a-chip model to determine the regulation of FKBPL and galectin-3 in preeclampsia[J]. Cellular and Molecular Life Sciences, 2023, 80(2): 44. |
| 115 | ROMBERG S I, KREIS N N, FRIEMEL A, et al. Human placental mesenchymal stromal cells are ciliated and their ciliation is compromised in preeclampsia[J]. BMC Medicine, 2022, 20(1): 35. |
| 116 | ARUMUGASAAMY N, ETTEHADIEH L E, KUO C Y, et al. Biomimetic placenta-fetus model demonstrating maternal-fetal transmission and fetal neural toxicity of zika virus[J]. Annals of Biomedical Engineering, 2018, 46(12): 1963-1974. |
| 117 | KARVAS R M, KHAN S A, VERMA S, et al. Stem-cell-derived trophoblast organoids model human placental development and susceptibility to emerging pathogens[J]. Cell Stem Cell, 2022, 29(5): 810-825.e8. |
| 118 | RAGER J E, BANGMA J, CARBERRY C, et al. Review of the environmental prenatal exposome and its relationship to maternal and fetal health[J]. Reproductive Toxicology, 2020, 98: 1-12. |
| 119 | MANANGAMA G, MIGAULT L, AUDIGNON-DURAND S, et al. Maternal occupational exposures to nanoscale particles and small for gestational age outcome in the French Longitudinal Study of Children[J]. Environment International, 2019, 122: 322-329. |
| 120 | MUOTH C, WICHSER A, MONOPOLI M, et al. A 3D co-culture microtissue model of the human placenta for nanotoxicity assessment[J]. Nanoscale, 2016, 8(39): 17322-17332. |
| 121 | SCHULLER P, ROTHBAUER M, KRATZ S R A, et al. A lab-on-a-chip system with an embedded porous membrane-based impedance biosensor array for nanoparticle risk assessment on placental Bewo trophoblast cells[J]. Sensors and Actuators B: Chemical, 2020, 312: 127946. |
| 122 | GINGRICH J, TICIANI E, VEIGA-LOPEZ A. Placenta disrupted: endocrine disrupting chemicals and pregnancy[J]. Trends in Endocrinology and Metabolism, 2020, 31(7): 508-524. |
| 123 | TICIANI E, PU Y, GINGRICH J, et al. Bisphenol S impairs invasion and proliferation of extravillous trophoblasts cells by interfering with epidermal growth factor receptor signaling[J]. International Journal of Molecular Sciences, 2022, 23(2): 671. |
| 124 | XU C K, MA H J, GAO F M, et al. Screening of organophosphate flame retardants with placentation-disrupting effects in human trophoblast organoid model and characterization of adverse pregnancy outcomes in mice[J]. Environmental Health Perspectives, 2022, 130(5): 57002. |
| 125 | YAMASHITA M, MARKERT U R. Overview of drug transporters in human placenta[J]. International Journal of Molecular Sciences, 2021, 22(23): 13149. |
| 126 | PEMATHILAKA R L, ALIMORADI N, REYNOLDS D E, et al. Transport of maternally administered pharmaceutical agents across the placental barrier in vitro [J]. ACS Applied Bio Materials, 2022, 5(5): 2273-2284. |
| 127 | RICHARDSON L S, KAMMALA K A, COSTANTINE M M, et al. Testing of drugs using human feto-maternal interface organ-on-chips provide insights into pharmacokinetics and efficacy[J]. Lab on a Chip, 2022, 22(23): 4574-4592. |
| [1] | CHEN Xiyue, WANG Yaqing, BAO Fang, QIN Jianhua. Advances in the application of liver on a chip in biomedical research [J]. Synthetic Biology Journal, 2024, 5(4): 813-830. |
| [2] | HONG Yuan, LIU Yan. Research progress of brain organoids in regenerative medicine [J]. Synthetic Biology Journal, 2024, 5(4): 754-769. |
| [3] | Qianwen CHEN, Siqi ZHAO, Yaojin PENG. Organoids: technological innovation and ethical controversies [J]. Synthetic Biology Journal, 2024, 5(4): 898-907. |
| [4] | HU Bowen, TAN Jiaping, LIU Xiaodong. Advances in the development of human embryo models [J]. Synthetic Biology Journal, 2024, 5(4): 719-733. |
| [5] | CAI Bingyu, TAN Xiangtian, LI Wei. Advances in synthetic biology for engineering stem cell [J]. Synthetic Biology Journal, 2024, 5(4): 782-794. |
| [6] | ZHANG Bohang, QI Xiaoxuan, YUAN Yan. Advancements in testicular organoids for in vitro spermatogenesis [J]. Synthetic Biology Journal, 2024, 5(4): 770-781. |
| [7] | HAN Yizhao, GUO Jia, SHAO Yue. Stem cell-based synthetic development: cellular components, embryonic models, and engineering approaches [J]. Synthetic Biology Journal, 2024, 5(4): 734-753. |
| [8] | Shikai LI, Dong′ao ZENG, Fangzhou DU, Jingzhong ZHANG, Shuang YU. The construction approaches and biomaterials for vascularized organoids [J]. Synthetic Biology Journal, 2024, 5(4): 851-866. |
| [9] | Ke’er HU, Hanqi WANG, Ruqi HUANG, Canyang ZHANG, Xinhui XING, Shaohua MA. Integrated design strategies for engineered organoids and organ-on-a-chip technologies [J]. Synthetic Biology Journal, 2024, 5(4): 883-897. |
| [10] | CHEN Ziling, XIANG Yangfei. Integrated development of organoid technology and synthetic biology [J]. Synthetic Biology Journal, 2024, 5(4): 795-812. |
| [11] | AI Zongyong, ZHANG Chengting, NIU Baohua, YIN Yu, YANG Jie, LI Tianqing. Early human embryo development and stem cells [J]. Synthetic Biology Journal, 2024, 5(4): 700-718. |
| [12] | Qian MENG, Cong YIN, Weiren HUANG. Tumor organoids and their research progress in synthetic biology [J]. Synthetic Biology Journal, 2024, 5(1): 191-201. |
| [13] | Liyu ZHU, Yulong ZHAO, Wei LI, Libin WANG. Progress in mammalian chromosome engineering [J]. Synthetic Biology Journal, 2023, 4(2): 394-406. |
| [14] | Can ZHANG, Liyang SHI, Jianwu DAI. Cultured meat from biomaterials: challenges and prospects [J]. Synthetic Biology Journal, 2022, 3(4): 676-689. |
| [15] | Chengzhi SONG, Yang SUN, Yi CAO. Effects of mechanical signals on stem cell fate determination [J]. Synthetic Biology Journal, 2022, 3(4): 781-794. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||